Translate this page into:
Association Between Source of Treatment and Quality of Childhood Diarrhea Management Among Under-Five Children in Nigeria
✉Corresponding author email: olorunsaiyec@arcadia.edu
Abstract
Background and Objective:
Despite the availability of low-cost and effective interventions, diarrhea remains one of the leading causes of under-five morbidity and mortality in Nigeria. We assessed the relationships between the source and quality of treatment for children with diarrhea in Nigeria.
Methods:
We analyzed cross-sectional data on 3,956 under-five children with a recent diarrheal episode, from the 2018 Nigeria Demographic and Health Survey. The outcome was quality of diarrhea management based on the administration of the following treatment recommendations: oral rehydration salt (ORS), zinc supplementation, increased oral fluids, and continued feeding. The exposure was the source of treatment (none; traditional/informal; public hospitals/health centers; private hospitals/clinics; and community-based services). Using adjusted, multivariable logistic regression, we estimated the odds ratio (OR) and 95% confidence intervals (CI) to predict the factors related to the quality of diarrhea management.
Results:
In all, only 1 in 5 children received all the four recommended diarrhea interventions. The odds of good quality diarrhea management were higher among children who received treatment in public hospitals/health centers, private hospitals/clinics, and community-based services compared to those of children who did not receive treatment (OR=2.52, 95% CI=1.89-3.34; OR=2.46, 95% CI=1.90-3.16; and OR=1.91, 95% CI= 1.40-2.59, respectively). Compared to children whose parents did not seek treatment, the odds of receiving ORS ranged from 2.1 times (OR: 2.11, 95% CI=1.44-3.11) for seeking care in traditional/informal sources to 12.3 times (95% CI=8.81-17.15) in public hospitals/health centers. We observed similar trends for zinc supplementation. The odds of increased oral fluids were higher in public and private hospitals/clinics (OR=1.44, 95% CI=1.03-2.01 and OR=2.08, 95% CI=1.57-2.76, respectively). Across all settings, the odds of continued feeding were significantly lower among children who received treatment compared to children who did not receive treatment.
Conclusion and Implications for Translation:
Our findings indicate poor quality diarrhea management across various treatment settings. Policies and programs that encourage caregivers to seek treatment and improve the quality of care may contribute to reducing childhood diarrhea-related morbidity and mortality in Nigeria.
Keywords
Childhood Diarrhea
Childhood Illnesses
Quality of Care
Under-Five Mortality
Nigeria
Introduction
Globally, 1.7 billion diarrheal illnesses occur each year resulting in more than half a million child deaths.1 Diarrheal illnesses and deaths are concentrated in sub-Saharan Africa and South Asia.2 Overall, in low-income countries, children less than three years old experience an average of three diarrheal episodes each year.1 In Nigeria, diarrhea is one of the leading causes of under-five morbidity and mortality.3 Recent studies have reported a national prevalence of childhood diarrhea of 12.6%, and sub-national prevalence as high as 21.1% in the northwest and 26.4% in the northeast regions of Nigeria.4-6 Risk factors for childhood diarrhea include lack of access to potable drinking water, poor sanitation and hygiene practices, suboptimal feeding practices, and malnutrition.2,7 Poor infrastructure including water, sanitation, and hygiene resources increases the susceptibility of children to diarrhea and has significant implications for child health and survival.8
Dehydration is a major complication associated with diarrhea and can result from the excessive loss of fluids and electrolytes in watery stools.1,8 Also, frequent or prolonged diarrheal episodes can lead to undernutrition, which in turn, increases a child's susceptibility to other serious infectious diseases and death.9 In 2004, the World Health Organization (WHO) and United Nations Children's Fund (UNICEF) recommended the following interventions for managing uncomplicated childhood diarrhea: oral rehydration salt (ORS), zinc supplementation, increased liquids to drink, and continued feeding with the same or more amount of food, in addition to consultation with a health care provider.10 Consultation with a health care provider, in a facility- or community-based setting, can help prevent harmful home-based practices and ensure prompt treatment for severe diarrhea and dehydration. Despite the availability of these simple, effective, and low-cost interventions, several children do not receive appropriate diarrhea treatment.11,12
Studies in Nigeria and elsewhere have established the important role of social and demographic factors in enabling access to and use of appropriate treatment for childhood diarrhea. Some of these factors include women's education, economic status, rural/urban residence, and ethnicity.4,12-15 Children whose mothers have lower socioeconomic status experience more barriers to optimal home-based management and care-seeking practices for diarrhea. Moreover, few studies have explored the quality of diarrhea management and findings have indicated generally suboptimal quality of care.11,12,14
Due to the significant burden of diarrhea on the health and survival of children in Nigeria and other under-resourced settings, it is pertinent to understand the sources and quality of treatment for children with diarrhea. Therefore, we aimed to assess the sources of care for children with diarrhea and the quality of treatment they received. The findings may contribute to quality improvement efforts across various health care settings, and policies and programs to ensure universal health coverage in the country.
Methods
Data and Study Sample
The data were from the 2018 Nigeria Demographic and Health Survey (DHS).16 The DHS is a crosssectional survey designed to provide social and health indicators at national and sub-national levels in participating countries. The survey methodology is described in detail elsewhere.16 To summarize, the survey employs a two-stage, stratified random sampling methodology. At the first stage, enumeration areas are selected from the most recent census. At the second stage, in each selected enumeration area, households are randomly selected from an updated list. In selected households, information on household characteristics and members is elicited from an eligible adult. Additionally, trained enumerators using paper and pencil methods, following the receipt of informed consent, administer questionnaires for women, children, and men. The survey is weighted for over-sampling of certain populations and nonresponse. Data were extracted from the children's recode file. We included data on under-5 children who had experienced at least one recent acute diarrheal episode (i.e., non-bloody diarrhea) in the two weeks preceding the survey. Children were excluded from the data if their caregiver responded, “don't know” to the question on a recent diarrheal episode or the source of treatment for the sick child. Therefore, the analytic sample was 3,956 under-5 children (Figure 1).
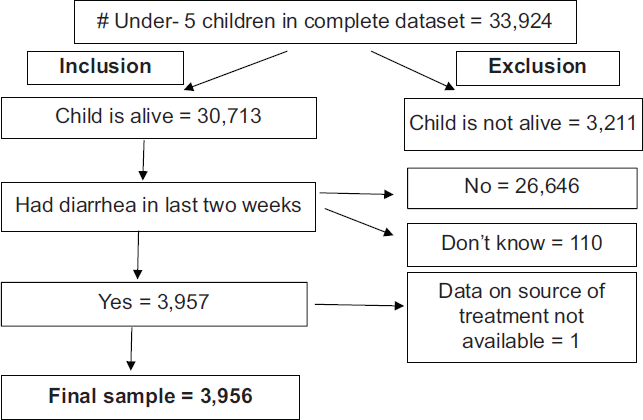
- Study sample showing inclusion and exclusion criteria.
Study Variables
The primary outcome was a composite variable, quality of diarrhea management. We defined the quality of diarrhea management as a child with a recent diarrheal episode receiving all four recommended interventions: 1) oral rehydration salt, 2) zinc supplementation, 3) increased fluid intake, and 4) continued feeding with the same or more amount of food as before the recent diarrheal episode.10 The variable was coded 1 (good quality) if the mother/caregiver reported that the child received all four interventions, otherwise it was coded 0 (poor quality). We also examined the four interventions independently as secondary outcomes, each coded 1 (yes) or 0 (no).
The exposure variable was the source of treatment. This was a categorical variable representing the source from which a mother/caregiver reported receiving treatment for the child. The variable was coded as follows: 1) no treatment (parent/caregiver did not seek treatment); 2) informal/traditional (traditional medicine practitioners, open markets, or itinerant medicine sellers); 3) public hospitals or health centers/clinics; 4) private hospitals or clinics; and 5) community-based services (public health post, public or private community health worker or mobile clinic, private pharmacy, or patent medicine store/chemist).
We selected covariates based on the existing literature. These included maternal education (none, primary, secondary, or higher), household wealth quintile (poorest, poor, middle, rich, richest), marital status (married, not married), residence (rural or urban), mother's ethnicity (Hausa/Fulani, Igbo, Yoruba, others), maternal age (15-19, 20-29, 30-39, 4049 years), and the number of under-5 children in the household.4,12-14,17 Other covariates were mother's knowledge of ORS (yes or no), frequency of mass media exposure (newspapers, TV, or radio - none, less than once a week, at least once a week), child's age (<6 months, 6-11 months, 12-23 months, 23-35 months, 36-59 months) and barriers to health care (financial, distance, waiting time, obtaining permission, or not having someone to go with - coded yes if the mother cited one or more barriers, or coded no).4,14,15,17,18
Statistical Analysis
We calculated frequencies of the sociodemographic characteristics of the study sample. We also computed the prevalence of healthcare-seeking and the diarrhea treatment interventions provided to children in the sample. From the covariates, we selected potential confounders for the multivariable logistic regression using Chi-Square and t tests to identify those that showed significant tests at P<0.15 level.19 Logistic regression models were constructed for the primary outcome, quality of diarrhea management, and each secondary outcome, based on the following formula: logit(p)=log[y/1-y] = b0 + b1X1 + b2X2 + b3X3 +... + b11X11 where p=probability of y to be 1, y=outcome; b0=the intercept; b1, b2, b3...b11=respective parameter values; X1, X2, X3...X11=values of up to the 11th of 11 respective explanatory variables. Each model was adjusted for potential confounders. Measures of associations were expressed as odds ratios (OR) and 95% confidence intervals (CI). We report our findings in compliance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies. All analyses were weighted and conducted in Stata version 15,20 using the ‘survey’ command to account for the complex survey design.
Ethics Approval
This study was a secondary analysis of publicly available data; therefore, institutional review board approval was not required. The Nigeria Health Research Ethics Committee and the ICF International Inc. Review Board reviewed and approved the DHS survey protocol.16 The DHS Program granted us access to the dataset following the submission of research aims.
Results
Descriptive Characteristics of Study Participants
Children aged 12-23 months composed 31.4% (1,229/3,956) of the sample, while 8.0% (324/3,956) were under 6 months old; 16.0% were 6-11 months (641/3,956); 20.4% were 24-35 months (800/3,956); and 24.1% were 36-59 months old (962/3,956) (Table 1). About 57.1% (2,248/3,956) of mothers had no formal education, 15.2% (614/3,956) had primary, 23.4% (931/3,956) had secondary, and 4.3% (163/3,956) had higher educational levels. Household wealth ranged from 31.2% (1,303/3,956) in the poorest quintile to 8.2% (294/3,956) in the richest. About 70.3% (2,858/3,956) of participants resided in rural areas. More than 4 in 10 mothers (42.9%; 1,794/3,956) had no exposure to mass media. About 87.3% (3,414/3,956) of mothers knew of ORS. More than one-half (56.2%; 2,220/3,956) of the women in the study experienced one or more barriers to seeking health care.
| Variable | Weighted % |
|---|---|
| Age (months) | |
| 0-5 | 8.0 |
| 6-11 | 16.0 |
| 12-23 | 31.4 |
| 24-35 | 20.4 |
| 36-59 | 24.1 |
| Maternal education | |
| None | 57.1 |
| Primary | 15.2 |
| Secondary | 23.4 |
| Higher | 4.3 |
| Household wealth | |
| Poorest | 31.2 |
| Poor | 26.6 |
| Middle | 19.6 |
| Rich | 14.3 |
| Richest | 8.2 |
| Residence | |
| Rural | 70.3 |
| Urban | 29.7 |
| Maternal age | |
| 15-19 | 6.6 |
| 20-29 | 51.7 |
| 30-39 | 33.3 |
| 40-49 | 8.5 |
| Ethnicity | |
| Hausa/Fulani | 59.3 |
| Igbo | 6.2 |
| Yoruba | 5.1 |
| Others | 29.4 |
| Current marital status | |
| Married/cohabiting | 95.7 |
| Not married | 4.3 |
| Media exposure | |
| None | 42.9 |
| Less than one a week | 21.3 |
| At least once a week | 26.8 |
| Mother's knowledge of ORS | |
| No | 12.7 |
| Yes | 87.3 |
| Barriers to health care seeking | |
| No | 43.8 |
| Yes | 56.2 |
| # Under-5 children in household (Mean [confidence interval]) | 2.32 [2.25, 2.39] |
ORS=oral rehydration salt
Sources and Quality of Diarrhea Treatment
The prevalence of recent diarrhea among under-5 children was 11.6% (3,957/30,713) (result not shown in tables). Mothers/caregivers of sick children who sought treatment from traditional/informal sources constituted 7.2% (286/3,956) of the sample. As well, 17.2% (643/3,956) sought treatment from public hospitals/clinics, 29.5% (1,143/3,956) from private hospitals/clinics, 13.8% (588/3,956) from community- based services, while 32.4% (1,296/3,956) of the mothers did not seek treatment (Table 2). About 41.9% (1,572/3,956) of the children received ORS, 31.1% (1,151/3,956) received zinc supplements, 14.2% (586/3,956) received increased liquids to drink, and 39.3% (1,638/3,956) continued to be fed with the same or more amount of food. Only 1 in 5 children (20.9%; 857/3,956) received all four recommended interventions (good quality diarrhea management).
| Variable | Weighted % |
|---|---|
| Sources of Treatment | |
| None | 32.4 |
| Traditional/informal | 7.2 |
| Public hospitals/health centers | 17.2 |
| Private hospitals/clinics | 29.5 |
| Community-based services | 13.8 |
| Received good quality diarrhea management | 20.9 |
| Received ORS | 41.9 |
| Received Zinc Supplement | 31.1 |
| Given increased fluids to drink | 14.2 |
| Feeding with same or more amount of food | 39.3 |
ORS=oral rehydration salt
Associations between Sources of Treatment and Quality of Diarrhea Management
The odds of receiving good quality diarrhea management were higher among children who received treatment in public hospitals/health centers (OR=2.52, 95% 0=1.89-3.36), private hospitals/clinics (OR=2.46, 95% 0=1.90-3.16), or from community-based sources (OR=1.91, 95% CI= 1.40-2.59), compared to those who did not receive treatment (Table 3). Compared to children whose parents did not seek treatment, children whose parents sought treatment had higher odds of receiving ORS (traditional/informal sources: OR=2.11, 95% CI=1.44-3.11; public hospitals/health centers: OR= 12.30, 95% CI=8.81-17.15; private hospitals/clinics: OR=3.86, 95% CI=3.07- 4.86; community-based services: OR=5.71, 95% CI=4.13-7.88). Compared to children whose parents did not seek treatment, children whose parents sought treatment had higher odds of receiving zinc supplementation (traditional/informal sources: OR=2.40, 95% CI=1.51-3.84; public hospitals/health centers: OR= 12.33, 95% CI=8.87-17.15; private hospitals/clinics: OR=4.76, 95% CI=3.42- 6.63; community-based services: OR=6.74, 95% CI=4.75-9.55). Children had higher odds of receiving increased fluids to drink when they got treatment from public or private hospitals/health centers (OR=1.44, 95% CI=1.03-2.01), or private hospitals/clinics (OR=2.08, 95% CI= 1.57-2.76) compared to children who did not receive treatment. The odds of continued feeding with the same or more amount of food were lower among children who received treatment compared to children who did not receive treatment (public hospitals/health centers: OR=0.49, 95% CI=0.37-0.63; private hospitals/clinics: OR=0.73, 95% 0=0.59-0.91; community-based services: OR=0.62, 95% CI=0.48-0.79; traditional/informal sources: OR=0.60, 95% CI=0.43-0.83).
| Variable | OR [95% CI] | ||||
|---|---|---|---|---|---|
| Good quality diarrhea management | ORS | Zinc Supplement | Increased fluids | Same or more food | |
| Source of treatment | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Traditional/informal | 1.47 [0.97, 2.21] | 2.11 [1.44, 3.11] | 2.40 [1.51,3.84] | 1.13 [0.72, 1.77] | 0.60 [0.43, 0.83] |
| Public hospital/clinic | 2.52 [1.89, 3.36] | 12.30 [8.81, 17.15] | 12.33 [8.87, 17.15] | 1.44 [1.03, 2.01] | 0.49 [0.37, 0.63] |
| Private hospital/clinic | 2.46 [1.90, 3.16] | 3.86 [3.07, 4.86] | 4.76 [3.42, 6.63] | 2.08 [1.57, 2.76] | 0.73 [0.59, 0.91] |
| Community-based | 1.91 [1.40, 2.59] | 5.71 [4.13, 7.88] | 6.74 [4.75, 9.55] | 1.19 [0.83, 1.70] | 0.62 [0.48, 0.79] |
| Maternal education | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Primary | 1.36 [1.04, 1.77] | 0.93 [0.72, 1.21] | 0.83 [0.63, 1.10] | 1.47 [1.06, 2.02] | 0.85 [0.66, 1.08] |
| Secondary | 1.14 [0.85, 1.52] | 0.67 [0.51,0.89] | 1.19 [0.86, 1.66] | 1.25 [0.92, 1.70] | 0.82 [0.60, 1.11] |
| Higher | 1.30 [0.78, 2.17] | 0.79 [0.45, 1.38] | 1.57 [0.89, 2.79] | 1.45 [0.80, 2.63] | 0.91 [0.55, 1.51] |
| Household wealth | |||||
| Poorest | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Poor | 0.75 [0.56, 1.02] | 1.06 [0.80, 1.40] | 0.91 [0.69, 1.20] | 0.78 [0.55, 1.10] | 0.80 [0.64, 1.01] |
| Middle | 1.78 [0.54, 2.10] | 1.20 [0.88, 1.63] | 1.49 [1.07, 2.08] | 0.66 [0.44, 1.00] | 1.09 [0.83, 1.42] |
| Rich | 1.72 [0.48, 2.07] | 1.43 [0.99, 2.08] | 1.55 [1.03, 2.34] | 0.69 [0.43, 1.09] | 0.95 [0.68, 1.32] |
| Richest | 1.95 [0.98, 2.57] | 2.17 [1.33, 3.52] | 1.37 [0.83, 2.28] | 0.88 [0.50, 1.55] | 1.19 [0.77, 1.83] |
| Residence | |||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Urban | 0.61 [0.45, 1.22] | 1.13 [0.87, 1.48] | 1.03 [0.77, 1.39] | 0.52 [0.36, 0.76] | 0.98 [0.77, 1.26] |
| Maternal age (years) | |||||
| 15-19 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 20-29 | 1.17 [0.78, 1.75] | 1.10 [0.74, 1.64] | 0.96 [0.60, 1.53] | 1.21 [0.78, 1.88] | 0.97 [0.72, 1.32] |
| 30-39 | 1.13 [0.74, 1.73] | 1.06 [0.71, 1.58] | 1.12 [0.67, 1.86] | 1.07 [0.67, 1.71] | 0.95 [0.68, 1.32] |
| 40-49 | 1.31 [0.81,2.15] | 0.86 [0.52, 1.42] | 1.00 [0.58, 1.75] | 1.45 [0.87, 2.42] | 1.00 [0.68, 1.46] |
| Ethnicity | |||||
| Hausa/Fulani | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Igbo | 2.11 [1.44, 3.12] | 1.50 [1.01, 2.26] | 0.54 [0.34, 0.87] | 2.56 [1.65, 3.97] | 2.67 [1.86, 3.84] |
| Yoruba | 1.56 [0.90, 2.70] | 1.13 [0.75, 1.70] | 0.56 [0.32, 0.99] | 1.70 [0.91,3.18] | 3.16 [1.98, 5.06] |
| Others | 1.44 [1.14, 1.82] | 1.16 [0.92, 1.47] | 0.64 [0.51,0.80] | 1.69 [1.25, 2.30] | 1.62 [1.28, 2.06] |
| # Children under-five years in the household | 0.98 [0.90, 1.06] | 0.99 [0.92, 1.06] | 0.97 [0.90, 1.04] | 0.97 [0.88, 1.08] | 0.98 [0.91, 1.05] |
| Media exposure | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Less than once/week | 1.28 [0.98, 1.68] | 1.14 [0.88, 1.49] | 1.22 [0.91, 1.63] | 1.14 [0.83, 1.56] | 1.35 [1.07, 1.71] |
| At least once/week | 1.85 [1.41,2.42] | 1.49 [1.17, 1.91] | 1.30 [0.98, 1.72] | 1.53 [1.08, 2.15] | 1.29 [1.04, 1.60] |
| Child's age (months) | |||||
| 0-5 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 6-11 | 1.12 [0.74, 1.72] | 1.07 [0.75, 1.53] | 1.48 [0.94, 2.35] | 1.36 [0.84, 2.19] | 0.90 [0.65, 1.24] |
| 12-23 | 1.46 [1.00, 3.13] | 1.42 [0.99, 2.02] | 1.56 [1.01,2.41] | 1.75 [1.12, 2.73] | 0.80 [0.58, 1.11] |
| 24-35 | 1.55 [1.03, 2.33] | 1.28 [0.90, 1.81] | 1.53 [1.01,2.33] | 1.71 [1.08, 2.73] | 1.37 [0.96, 1.94] |
| 36-59 | 1.43 [0.95, 2.17] | 1.10 [0.76, 1.58] | 1.43 [0.93, 2.21] | 1.60 [0.98, 2.61] | 1.22 [0.87, 1.72] |
| Mother's knowledge of ORS | |||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.35 [0.99, 1.88] | 20.04 [11.62, 34.55] | 2.64 [1.79, 3.88] | 0.94 [0.67, 1.31] | 1.16 [0.89, 1.50] |
| Barriers to health care seeking | |||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.06 [0.89, 1.26] | 0.80 [0.67, 0.95] | 0.91 [0.75, 1.09] | 1.18 [0.95, 1.46] | 1.08 [0.91, 1.28] |
OR=odds ratio, ORS=oral rehydration salt.
Discussion
Good quality diarrhea management is cost-effective and contributes to child survival. We assessed the relationships between the sources and quality of treatment for acute childhood diarrhea in Nigeria, according to WHO recommendations.10 We extend the research on treatment for childhood diarrhea by using the most recent nationally representative data to explore variations in the quality of care across different treatment settings. We are not aware of any study that included community-based services as an independent category among the sources of treatment, as a possible predictor of the quality of diarrhea management in Nigeria.
Maternal education, ethnicity, household wealth, rural/urban residence, child's age, use of public media, and barriers to health care predicted the quality of treatment. These are known determinants of child survival in Nigeria.21 Moreover, most caregivers/mothers in our study resided in rural locations, more than one-half had no education, and nearly 6 in10 were of Hausa/Fulani ethnicity. A previous study found higher rates of under-five mortality in these groups.22 Hence, contextual and individual factors remain an important issue in care-seeking for childhood illnesses and should be addressed. The sources of treatment ranged from informal/traditional services to the formal health system (i.e., community-based services, private, or public health facilities). Private hospitals/clinics were the most common sources of treatment. A recent study in Ethiopia revealed that two-thirds of mothers/caregivers sought treatment for child diarrhea outside the home.23 However, contrary to our findings, most caregivers in the Ethiopia study sought care from public health facilities.
Similar to a prior study, treatment provided in public health facilities was associated with better quality.23 Besides, we observed comparable odds of good quality treatment in private health facilities. In many low-resource settings, public health facilities provide a higher quality of care than private facilities.24 In another study, adequate diarrhea management was most likely to occur in health facilities or when treatment was provided by community health workers.11 The decision to seek treatment at a health facility is related to distance, place of residence, and perceived quality.14 Public and community-based facilities are typically closer to communities, hence, more convenient and accessible to families. However, in Nigeria, due to frequent stock-out of medicines and supplies, and other health system challenges, private health facilities are commonly used as a reliable but more expensive alternative to public facilities.25 This may be partly responsible for the comparable quality of treatment in public and private health facilities in our study.
The odds of a sick child receiving ORS and zinc supplements were higher in public health facilities, followed by community-based services (health posts, community health workers, etc.). The greater odds of ORS provision at public hospitals/clinics could be due to recent interventions promoting the production and supply of ORS and zinc for the public and private sectors in some Nigerian states.26 An evaluation of this program revealed that ORS was provided more frequently in public hospitals/clinics followed by community-based settings, private facilities, and traditional/informal sources.26 Additional efforts are needed to promote the recommendation and uptake of ORS in all settings that treat sick children. In recent efforts that achieved an 85% increase in ORS use in Sierra Leone, deliberate steps taken included maintaining the supply chain for ORS at every level, community- based distribution, and abolishing healthcare costs for pregnant women and under-5 children. These steps contributed to strengthening the health system and addressing contextual barriers to quality care.11 Similar steps may be necessary to achieve a rapid scale-up of ORS use in Nigeria.
We found comparable odds of zinc supplementation as ORS across all sources of treatment. The provision of zinc supplementation for diarrhea management has increased compared to previous studies.11,14 The increased inclusion of zinc in childhood diarrhea treatment at health facilities may also be linked to recent in-service training of health workers.27 Zinc supplementation in traditional/informal sources of care was limited, possibly due to their exclusion from the formal health system and available training opportunities. Contrary to recent findings from Ethiopia, our results suggest that maternal education, media exposure, and the number of under-5 children in a household were not associated with zinc supplementation.28 More than 40% of women in the current study had no media exposure; hence, this may be a possible reason for our findings. Nonetheless, these results warrant further investigation.
Increased fluid intake in children was the least practiced recommended intervention; however, this outcome showed a slight increase compared to findings from a previous study in Nigeria.14 The odds of increased fluid intake among sick children were high when treatment was received in private health facilities, followed by that in public health facilities. Other population-based, cross-sectional studies of mothers of under-5 children have reported reduced fluid intake during diarrheal episodes as a common practice among caregivers, mostly due to poor knowledge of nutritional management during childhood diarrhea, and lack of awareness of the possibility of dehydration.7,29 The misconception that increasing oral fluids during a diarrheal episode causes increased watery stools could be a possible reason for this finding, as noted in the existing literature.30 Thus, the education of caregivers and community-based service providers would help address this knowledge gap.
Surprisingly, we found that the odds of the caregiver continuing to feed a sick child with the same or more amount of food were significantly lower among those who sought treatment compared to those who did not. Contrary to our findings, a study in Sudan found increased feeding during childhood diarrheal episodes.31 Children taken to the health facility for treatment may have more severe illness and, thus, may be unable to feed. Another possible reason for this finding could be discordance between policy and practice whereby health care providers may not be effectively counseling parents/caregivers to continue feeding the sick child, as recommended in treatment guidelines.29 A 2014 clinic-based, cross-sectional study determined the perception, knowledge, and practice of home management of diarrhea among caregivers of under-5 children in southern Nigeria.32 That study's findings showed that the perception of caregivers about food quality and quantity influenced continued feeding during diarrheal episodes. Thus, caregivers may be unknowingly withholding food from the sick child due to these misconceptions.32
Strengths and Limitations
A key strength of this study is the analytic approach of examining an overall index of quality of diarrhea management and each intervention, independently, across the different sources of treatment. This approach extends our understanding of areas where the health system is performing well and areas of potential improvement in the management of acute childhood diarrhea, a leading cause of under-five morbidity and mortality in Nigeria. Further, the use of recent, nationally representative data, provides an up-to-date snapshot of the quality of care for children with diarrhea. This information can help policymakers and program managers develop priorities and plan interventions that can potentially reduce the morbidity and mortality associated with childhood diarrhea in Nigeria.
Our study also has some limitations. First, the data are based on self-reported care-seeking behaviors and treatment interventions. Recall bias may affect the quality of the information provided by caregivers. However, limiting the recall period to two weeks before the survey should have greatly reduced this bias. Second, our analysis was limited to the variables that were available in the dataset. Notably, we could not account for cultural beliefs and practices that may affect caregivers' health-seeking behaviors and treatment practices. Third, the data also did not include variables on health system barriers to the appropriate treatment of sick children. Examples of such variables may include stock-outs of medicines, availability of trained health care providers, and the cost of treatment. Qualitative studies involving caregivers of under-5 children and health care providers can aid our understanding of cultural and health system influences on diarrhea management.
Conclusion and Implications for Translation
Across all the settings where parents/caregivers sought treatment, we found overall poor quality of care, with only 1 in 5 children receiving good quality treatment for diarrhea; these results are generalizable to Nigeria. Of the four key interventions in the WHO guidelines,10 ORS was the most frequently provided treatment for diarrhea. There is room for improvement in the use of these cost-effective solutions for addressing one of the leading causes of under-five deaths in Nigeria. There is a dire need for quality improvement programs and increased in-service support for health care providers. Training and job aids may be helpful first steps. One-third of the caregivers in our study did not seek treatment. Thus, there are opportunities to raise awareness across the country on the need to seek treatment for diarrhea and to promote integrated community case management of childhood illnesses. Further, with nearly 6 in 10 caregivers in our study reporting that they had some access to mass media, program managers and policymakers can provide localized public service announcements on diarrhea management in the predominant local languages in different parts of the country.
Compliance with Ethical Standards
Conflicts of interest:
The authors have no conflicts of interest to disclose.
Financial Disclosure:
The authors have no relevant financial interests to disciose.
Ethics Approval:
This study was a secondary analysis of publicly available data; therefore, institutional review board approval was not required. The Nigeria Health Research Ethics Review Committee and the ICF International Inc. Review Board reviewed and approved the DHS survey protocol. The DHS Program granted us access to the dataset following the submission of research aims.
Disclaimer:
The publication of this article was supported by the Global Health and Education Projects, Inc. (GHEP) through the Emerging Scholar's Grant Program (ESGP). The information, contents, and conclusions are those of the author(s) and should not be construed as the official position or policy of, nor should any endorsements be inferred by ESGP or GHEP
Acknowledgments:
The authors thank Ms. Kylie Reinhart, a BSPH student at Arcadia University, for her assistance with the literature review for an earlier manuscript draft.
Funding/Support:
No funding was received for conducting this study.
References
- Diarrheal Disease. World Health Organization; Published May 2, 2017 (accessed )
- Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17(9):909-948.
- [CrossRef] [PubMed] [Google Scholar]
- Direct estimates of cause-specific mortality fractions and rates of under-five deaths in the northern and southern regions of Nigeria by verbal autopsy interview. PloS One. 2017;12(5):e0178129.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and determinants of diarrhoea among infants in selected primary health centres in Kaduna north local government area, Nigeria. Pan Afri Med J. 2017;28(1):109.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal education and diarrhea among children aged 0-24 months in Nigeria. Afr J Reprod Health. 2017;21(3):27-36.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of childhood diarrhea among under-five year old children in Nigeria: A population-based study using the 2013 demographic and health survey data. Turk J Pediatr. 2018;60(4):353-360.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding careseeking for child illness in sub-Saharan Africa: a systematic review and conceptual framework based on qualitative research of household recognition and response to child diarrhoea, pneumonia and malaria. Soc. Sci Med. 2013;86:66-78.
- [CrossRef] [PubMed] [Google Scholar]
- Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet. 2013;381(9875):1417-1429.
- [CrossRef] [PubMed] [Google Scholar]
- Global burden of childhood pneumonia and diarrhea. Lancet. 2013;381(9875):1405-1416.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Management of Acute Diarrhea: WHO/UNICEF Joint Statement. World Health Organization; Published 2004 (accessed )
- Diarrhea management in children under five in sub-Saharan Africa: does the source of care matter? A Countdown analysis. BMC Public Health. 2016;16(1):830.
- [CrossRef] [PubMed] [Google Scholar]
- Careseeking for childhood diarrhoea at the primary level of care in communities in Cross River State, Nigeria. J Epidemiol Glob Health. 2016;6(4):303-313.
- [CrossRef] [PubMed] [Google Scholar]
- Management of children's acute diarrhea by community pharmacies in five towns of Ethiopia: simulated client case study. Ther Clin Risk Manag. 2016;12:515-26.
- [CrossRef] [PubMed] [Google Scholar]
- Diarrhoea management practices and child health outcomes in Nigeria: Sub-national analysis. Adv Integr Med. 2018;5(1):15-22.
- [CrossRef] [Google Scholar]
- Exploring health care seeking knowledge, perceptions and practices for childhood diarrhea and pneumonia and their context in a rural Pakistani community. BMC Health Serv Res. 2018;18(1):44.
- [CrossRef] [PubMed] [Google Scholar]
- Nigeria Demographic and Health Survey 2018 - Final Report. Abuja, Nigeria: NPC and ICF; Published 2019 (accessed )
- Mothers' knowledge, attitude and practice towards the prevention and home-based management of diarrheal disease among under-five children in Diredawa, Eastern Ethiopia, 2016: a cross-sectional study. BMC Pediatr. 2018;18(1):358.
- [CrossRef] [Google Scholar]
- Prevalence of diarrhea and associated risk factors in children under five years of age in Northern Nigeria: a secondary data analysis of Nigeria demographic and health survey 2013. In: Unpublished Master's Degree Project. Uppsala Universitet; 2017.
- [Google Scholar]
- Introduction to the Logistic Regression Model: Applied Logistic Regression (2nd). Wiley; 2000.
- [CrossRef] [PubMed]
- Stata Statistical Software: Release 15. In: [computer program]. TX: StataCorp LLC; 2017. College Station
- [Google Scholar]
- An examination of the maternal social determinants influencing under-5 mortality in Nigeria: Evidence from the 2013 Nigeria Demographic Health Survey. Glob Pub Health. 2017;12(6):744-756.
- [CrossRef] [PubMed] [Google Scholar]
- Association between ethnicity and under-5 mortality: analysis of data from demographic surveys from 36 low-income and middle- income countries. Lancet Glob Health. 2020;8(3):e352-e361.
- [CrossRef] [PubMed] [Google Scholar]
- Utilization of health facilities and predictors of healthseeking behavior for under-five children with acute diarrhea in slums of Addis Ababa, Ethiopia: a community-based cross-sectional study. J Health Popul Nutr. 2017;36(1):1-12.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing the choice of health care providing facility among workers in a local government secretariat in south western Nigeria. Ann Ib Postgrad Med. 2013;11(2):87-95.
- [Google Scholar]
- Distribution of health facilities in Nigeria: implications and options for universal health coverage. Int J Health Plan Manage. 2018;33(4):e1179-e1192.
- [CrossRef] [PubMed] [Google Scholar]
- Program evaluation of an ORS and zinc scale-up program in 8 Nigerian states. J Glob Health. 2019;9(1):010502-010513.
- [CrossRef] [PubMed] [Google Scholar]
- Private health care market shaping and changes in inequities in childhood diarrhoea treatment coverage: evidence from the analysis of baseline and endline surveys of an ORS and zinc scale-up program in Nigeria. Int J Equity Health. 2021;20(1):88.
- [CrossRef] [PubMed] [Google Scholar]
- Zinc utilization and associated factors among under-five children with diarrhea in East Africa: A generalized linear mixed modeling. Plos One. 2020;15(12):e0243245-e0243255.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and belief of nursing mothers on nutritional management of acute diarrhoea in infants, Ibadan, Nigeria. Afr J Food Agric Nutr. 2010;10(3):2291-2304.
- [CrossRef] [Google Scholar]
- Diarrheal management approach among caregivers of under-5-year- old children in an Egyptian rural area. Menoufia Med J. 2020;33(1):5-10.
- [CrossRef] [Google Scholar]
- Awareness and attitude towards dehydration and its management amongst mothers and factors influence on in under-five children of Omdurman locality, Sudan. Sudan J. Paediatr. 2020;20(2):136-143.
- [CrossRef] [PubMed] [Google Scholar]
- Home management of diarrhoea by caregivers presenting at the diarrhoea training unit of a tertiary hospital in Southern Nigeria. J. Adv Med 2014:5524-5540.
- [CrossRef] [Google Scholar]





