Translate this page into:
HIV Prevention in sub-Saharan Africa: Where Are Adolescents in the Continuum?
✉Corresponding author email: earmstrongmensah@gsu.edu
Abstract
The human immunodeficiency virus (HIV) is the leading cause of death among adolescents in sub-Saharan Africa and the second leading cause of death among adolescents globally, yet this population is not expressly targeted in HIV prevention. Consequently, HIV prevalence among this population continues to rise. In 2014, McNairy and El-Sadr developed and proposed an HIV prevention continuum framework to ensure zero HIV infection among HIV uninfected people. While a step in the right direction, the continuum does not categorically focus on adolescents and thus, does not include mechanisms to offset the potential challenges this population experiences in HIV prevention. Intentionally involving adolescents in HIV prevention is crucial, as this population is considered integral to achieving the Sustainable Development Goal 3.3 target of eliminating HIV by 2030. This paper examines the challenges of adolescent participation in HIV prevention in sub-Saharan Africa using the McNairy and El-Sadar HIV prevention continuum framework as a backdrop.
Keywords
HIV/AIDS
Adolescent
HIV Prevention
HIV Testing
Stigma •Pre-exposure Prophylaxis
SSA
Introduction
As of 2019, about 1.7 million people were newly infected with the human immunodeficiency virus (HIV), approximately 38 million were living with HIV, and an estimated 690,000 died from acquired immunodeficiency syndrome (AIDS) related causes globally.1 While HIV prevalence has significantly decreased in developed countries, the same cannot be said of most developing countries, especially those in sub-Saharan Africa (SSA). Inhabited by about 16 % of the world's population, SSA accounts for over two-thirds of all the people living with HIV, with countries in Eastern Africa (Kenya, Tanzania, Uganda) and Southern Africa (Botswana, Lesotho, Malawi, South Africa, Swaziland) bearing over 50% of the burden. Home to only 5% of the world's population, Eastern and Southern Africa account for over 60% of all children and adolescents (0-19 years) living with HIV globally.2
In the attempt to keep the fight against HIV on the global agenda, several international initiatives, including the Millennium Development Goals, the Sustainable Development Goals, the All In to End the Adolescent AIDS Epidemic Strategic Framework, and the Joint United Nations Program on HIV/AIDS (UNAIDS) 90-90-90 strategy, have been initiated.
Additionally, HIV prevention frameworks, including that by McNairy and El-Sadr, have also been developed and proposed. While these efforts have contributed to reducing HIV prevalence, they have focused primarily on adults and children. This paper examines the challenges of adolescent (People aged 10-19 years) participation in HIV prevention in developing countries using the McNairy and El-Sadr HIV prevention continuum (HPC) framework as a backdrop.
Adolescent HIV Risk Factors
Perinatal and sexual factors predispose adolescents to HIV. In SSA, adolescents who do not acquire HIV perinatally often do so through sexual activity. The non-personalized threat of HIV, early sexual debut, and the engagement in risky sexual behaviors such as the non-utilization of condoms during sexual activity, increase adolescent risk for HIV. Between 2008 and 2009, about 12 % of adolescent girls and 22% of adolescent boys in Kenya reported having had sex at the age of 15.3 In 2014, about 30% of adolescent boys and girls in the Central African Republic, and 30% of adolescent boys in Malawi and Lesotho indicated they engaged in their first sexual intercourse before the age of 15.4 In Ghana, by age 15,47% of adolescent boys and 38% of the adolescent girls had had sex.5
HIV/AIDS Burden Among Adolescents
According to UNAIDS, South Africa, Nigeria, Kenya, India, and Tanzania account for 50% of all adolescents living with HIV globally.6 In 2012, 300,000 of the 2.3 million new global HIV infections that occurred were among adolescents aged 15-19.7 Approximately 67% of the new infections globally were among adolescent girls in SSA – 82% in South Africa, 85% in Sierra Leone, and 89% in Gabon. The disproportionate prevalence of HIV among adolescent girls in SSA may be attributed to violence, unequal power relations with men, early marriage, socio-economic and cultural factors.8
The HIV Prevention Continuum
In 2014, McNairy and El-Sadar developed and proposed the HPC as a strategy for HIV prevention (Figure 1). Akin to the HIV care continuum, the HPC begins with HIV testing, followed by the linkage of HIV-negative persons to HIV prevention services such as access to pre-exposure prophylaxis (PrEP), voluntary medical male circumcision, and condoms. The third step is the retention of HIVnegative persons in HIV services such as counseling, psychosocial and outreach services, and the final step focuses on the adherence of HIV-negative persons to HIV prevention interventions, such as repeated HIV testing.9 According to McNairy and El-Sadr, to attain the global goal of zero new HIV infections, persons at risk for HIV have to avail themselves of all the steps along the path of the HPC.9
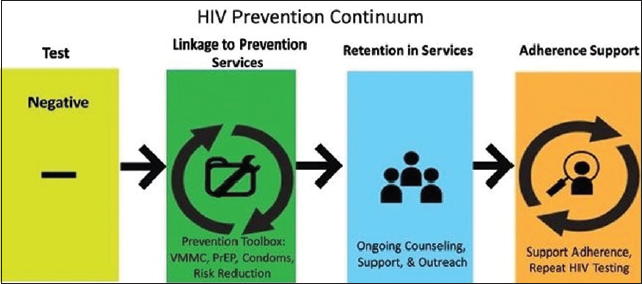
- McNairy-El-Sadr HIV Care and Prevention Continuum.9
Adolescents and the HIV Prevention Continuum
The goal of the McNairy-El-Sadr HPC is to ensure that persons at risk for HIV remain free of the disease. While a step in the right direction, the continuum is generic. It fails to recognize that populations at risk for HIV span various age ranges, including adolescents. As a result, the framework neglects to factor in mechanisms to offset the potential and peculiar challenges adolescents might experience at various steps of the proposed continuum.
HIV Testing
The McNairy-El-Sadr HPC highlights the need for HIV counseling and testing (HCT) as a gateway to HIV prevention, yet it does not include a mechanism to promote adolescent HIV testing. In many developing countries including those in SSA, the legal age at which a person can give consent for HIV testing is between 18 and 21 years. The need for parental or guardian consent for testing, the perceived negative reactions from parents and guardians, the lack of access to confidential testing, and the fear of HIV-related stigma, negatively affect adolescent HIV testing uptake. Long wait times, location and distance to HIV testing sites, time of service delivery, and the cost of services also serve as additional challenges to adolescent participation in HIV testing. In their 2014 study on patterns of HIV prevalence and testing among adolescents in SSA, Idele et al. found that less than 33 % of adolescents had ever been tested for HIV.4 In a cross-sectional study conducted in 2018, Ssebunya et al. also found that of the 1,439 adolescents aged 10-19 years living in seven districts in Uganda, only 13% of girls and 9% of boys had ever tested for HIV and received their results in the last 12 months.10 In another cross-sectional study conducted in 2016, of 23,367 adolescents in the Congo, Mozambique, Nigeria, and Uganda, Asaolou et al. found that only 27 % of adolescents aged 15 to 19 years had tested for HIV.11
To make the HIV testing component of the McNairy-El-Sadr HPC relevant to adolescents, the governments of SSA countries need to review their age policies on HIV consenting and testing, (as doing this will remove barriers and increase adolescent HIV testing uptake), designate specific facilities to provide HIV prevention services to adolescents efficiently and free of charge, and ensure that the designated facilities operate at times that are convenient for adolescents and are located where adolescents can easily access them.
Linkage to HIV Prevention Services
The second component of the McNairy-El- Sadr HPC focuses on linking people who are HIV negative to HIV prevention services such as condoms, pre-exposure prophylaxis (PrEP), and sexual and reproductive health (SRH) risk reduction information and education. Yet again, the HPC does not indicate how such services should be made available to adolescents. In SSA, where strict social norms, perceptions, and the stigma associated with adolescent sexual activity exist, adolescents often lack access to condoms. Thus, in a national survey conducted in South Africa, 43% of male adolescents and 45 % of female adolescents reported not having used a condom in their most recent sexual activity (Table 1).12 In another survey conducted in 32 sub-Saharan countries, only 38% of sexually active adolescent girls reported condom use during their last sexual encounter compared to 51% of adolescent boys.
| Total | Gender | Age Group | Gender by Age Group | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 15-19 | 20-24 | Male Age Group | Female Age Group | |||||
| 15-19 | 20-24 | 15-19 | 20-24 | |||||||
| Asked of those who report having had sexual intercourse: the last time you had sexual intercourse, did you use a condom? | Yes | 52% | 57% | 48% | 56% | 50% | 57% | 57% | 55% | 44% |
| No | 48% | 43% | 52% | 44% | 50% | 43% | 43% | 45% | 56% | |
| Total | 7692 | 3626 | 4066 | 3501 | 4191 | 1760 | 1866 | 1741 | 2325 | |
Source: Reproductive Health Research Unit. HIV and sexual behavior among young South Africans: a national survey of 15-24-year-olds.13
Despite its efficacy, most adolescents in SSA have no knowledge of PrEP. Indeed, a study conducted in SSA revealed that only 27% to 38 % of adolescents had ever heard of PrEP and only 1 to 1.5 % had ever used PrEP.13 In SSA countries (South Africa, Kenya, and Zimbabwe) where adolescents are familiar with the medication, clinicians are unwilling to prescribe it for adolescents.
Adolescents have unique HIV prevention needs, thus, they need to have access to HIV prevention medications and be involved as equal but distinct partners in the development and design of appropriate and effective HIV prevention interventions that meet their needs.
Retention in HIV Prevention Services
The retention of adolescents in HIV prevention services is a challenge in SSA that was not considered in the McNairy-El-Sadr HPC. Many adolescents in SSA find HIV prevention services unappealing. The unfriendly behavior of healthcare workers and their negative attitude towards adolescents who engage in sexual activity under the national age of consent, who are involved in same-sex relationships, and who use drugs, deter adolescents from going for routine sexually transmitted infection or HIV testing.
To address this challenge, healthcare workers in SSA need to be trained to provide HIV prevention services to adolescents without being judgmental and to treat adolescents with respect, tolerance, compassion, privacy, and confidentiality.
Adherence Support
While adherence to repeated HIV testing and the daily taking of PrEP as proposed by the McNairy- El-Sadr HPC is critical to HIV prevention, they are considered daunting activities by most adolescents. At a young age, adolescents still need a push, some guidance, and support to be adherent. To address this challenge, healthcare providers, parents, and guardians need to assess adolescent adherence practices, identify the factors that influence nonadherence, and come up with age-appropriate strategies to address the issues.
Conclusion and Implications for Translation
While the McNairy-El-Sadr HPC is a good framework for HIV prevention, it fails to include mechanisms that focus on adolescents. Identifying the express HIV prevention needs of adolescents, integrating adolescent developmental factors into the overall context of HIV prevention, and removing barriers to participation are critical to providing HIV prevention interventions and services that work for adolescents.
Compliance with Ethical Standards
Conflicts of interest:
The authors declare no competing interests.
Financial Disclosure:
Nothing to declare.
Ethics Approval:
Not Applicable.
Disclaimer:
None.
Acknowledgments:
None.
Funding/Support:
There was no funding for this study.
References
- New antiretroviral treatment for HIV. infect Dis Ther. 2016;5(3):329-352.
- [CrossRef] [PubMed] [Google Scholar]
- HiV and AIDS. UNICEF; Published 2016 (accessed )
- Kenya Demographic and Health Survey 2008-09. KNBS and ICF Macro; Published June 2010 (accessed )
- Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immune Defic Syndr. 2014;66(Suppl 2):S144-S153.
- [CrossRef] [PubMed] [Google Scholar]
- Adolescent Sexual And Reproductive Health in Ghana: A Synthesis of Research Evidence. In: Occasional Report. The Alan Guttmacher Institute; 2004. No. 13
- [Google Scholar]
- All in to End AIDS. UNAIDS; Published 2015 (accessed )
- UNICEF Analysis of UNAiDS 2012 HiV and AIDS Estimates. New York, NY: UNICEF; 2013.
- Health risk behaviour among adolescents living with HIV in sub-Saharan Africa: a systematic review and meta-analysis. Biomed Res int. 2018;2018:7375831.
- [CrossRef] [PubMed] [Google Scholar]
- A paradigm shift: focus on the HIV prevention continuum. Clin Infect Dis. 2014;59(Suppl 1):S12-S15.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and correlates of HIV testing among adolescents 10-19 years in a post-conflict pastoralist community of Karamoja region, Uganda. BMC Public Health. 2018;18(1):612.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of HIV testing among youth in sub-Saharan Africa: a cross-sectional study. PloS One. 2016;11(10):e0164052.
- [CrossRef] [PubMed] [Google Scholar]
- HIV and Sexual Behaviour Among Young South Africans: A National Survey of 15-24 Year Olds. Joint publication of Reproductive Health Research Unit and Love Life; 2004.
- Adolescent pre-exposure prophylaxis for HIV prevention: current perspectives. Adolesc Health Med Ther. 2017;8:137-148.
- [CrossRef] [PubMed] [Google Scholar]





