Translate this page into:
Body Mass Index and Breast Cancer Risks Among Igbo Women in Imo and Abia States, Nigeria: A Case Control Study
✉Corresponding author email: Chriswebren@gmail.com
Abstract
Background:
The association between body mass index (BMI) and breast cancer risk has been well recognized. The purpose of this study was to determine the association of BMI with breast cancer risks among women of Igbo origin in Imo and Abia states in South Eastern Nigeria.
Methods:
The study was conducted at three different locations: Abia State University Teaching Hospital Aba, Abia State; Federal Medical Centre, Owerri, Imo State; and the Maranatha Specialist Mission Hospital, Aba, Abia State. This was a prospective hospital-based case control study. Data were collected on socio-demographic characteristics and anthropometric measures using a structured questionnaire. Collected data were imported to SPSS version 23 for analysis. In all, 681 patients participated in the study of which 347 were cases and 334 were controls. The T-test was used to assess statistical differences of height, weight, and BMI in the studied groups. Logistic regressions were used to calculate the multivariate odds ratio (OR) using 95% confidence interval (CI) with significant level set at p>0.05.
Results:
Higher BMI is associated with increased risk of breast cancer. There was a significant statistical difference between the height of cases and controls in both pre-and post-menopausal women. The mean value of height was 161.14± 7.1cm among cases compared to controls which was 161.39 cm (p<0.05). The mean weight among cases was 66.34 ± 11.8kg compared to controls at 65.45 ± 9.2kg (p<0.05); the mean BMI was 25.6± 4.8kg/m2among cases compared to controls 25.l± 4.6 kg/m2 (p<0.05).
Conclusion and Implications For Translation:
Primary prevention measures are important to modestly curtail the increasing burden of obesity and high BMI. By controlling the weight, through physical activities, changes in diet and modestly alcohol intake will reduce the risk of breast cancer.
Keywords
Breast Cancer
Imo State
Abia State
South East Nigeria
Body Mass Index
Nigeria
Introduction
Background of the Study
Breast cancer is predominantly a disease of women and has a major impact on their health. Globally breast cancer accounts for 25.1% of all cancers in women ranking second (11.9%) overall when both sexes are considered together.1
Body Mass Index (BMI) is the weight in kilograms divided by the square of height in meters. BMI is a marker for general adiposity.2 BMI is categorized into underweight (BMI< 18.5kg/m2), normal range (18.5 – 24.9kg/m2), overweight (25- 30kg/m2), and obese (BMI> 30kg/m2) as defined by World Health Organization (WHO) BMI classification.3 In Nigeria, there are scanty studies on the association between breast cancer and BMI. The studies by Adebamowo et al4 and Ogundiran et al5,6 were done at the South Western part of Nigeria and there are no similar studies conducted in the South Eastern part of Nigeria. Result of the study done by Adebamowo et al4 shows that there is no association between obesity and breast cancer risk.
In other parts of the world specifically Europe, USA, and Australia, many epidemiological studies have shown that obesity is associated with a significantly elevated breast cancer risk.78 High BMI appears to be associated with increased breast cancer risk in post-menopausal women while it has slightly protective effect on pre-menopausal women.9,10 Considering the fact that there are limited studies on breast cancer risk and BMI association in Nigeria and none among Igbo women in Abia State and Imo State, this study became imperative to look at the association between BMI and breast cancer risk among the Igbo women.
According to the predictions made by Ferlay et al11 and Bray et al1, there would be 52,728 female breast cancers in Nigeria in 2035 accounting for about 25% of all female cancers. Among the three population based cancer registries established in Nigeria, breast cancer of the females top the list of cancers at Ibadan, Oyo State; Abuja, Federal Capital Territory; and Calabar, Cross River State. The risk of developing breast cancer is associated with several factors such as increasing age, family history, exposure to female reproductive hormones (both endogenous and exogenous), dietary factors, benign breast disease, environmental factors, early age at menarche, nuliparity or late age at first delivery, late age at postmenopausal, obesity and postmenopausal hormone therapy.12
Objectives of the Study
The study was designed to determine the association between BMI and breast cancer risk among Igbo women living in Abia and Imo States, Nigeria. We define risk factors of breast cancer as factors that increase the risk of breast cancer. These include age, family history, medical history, weight, physical activities, diet, smoking, exposure to estrogen, stress, anxiety, and alcohol consumption, among others.
Specific Aims and Hypothesis
Specific Aims: Our specific aims were to:
1) Determine the association between BMI and premenopausal breast cancer risks; 2) Determine the association between BMI and postmenopausal breast cancer risks; 3) Determine the association between height and breast cancer risks; and 4) Determine the association between weight and breast cancer risks for pre- and postmenopausal women.
Research Hypotheses: We posed the following research hypotheses:
There is no significant association between BMI and breast cancer risk among pre- menopausal women;
There is no significant association between BMI and breast cancer risk among postmenopausal women;
There is no significant association between height and breast cancer risk among women; and that
There is no significant association between weight and breast cancer risk among women in the study.
Methods
The study was a prospective hospital based case-control study conducted between October 2014 and August 2016. Information on exposure factors was collected from all the confirmed and suspected cases of breast cancer during the period; cases confirmed microscopically to have malignancy were included in the study. Frequency match was used for age and BMI. The data were collected for two years. Pre-designed case and control registration forms were used to collect the information. There was anthropometry measurement. Control was collated at the same hospitals.
Study Population
The study population was premenopausal and postmenopausal Igbo women attending Abia State University Teaching Hospital, Aba; the Maranatha Specialist Hospital, Aba; and Federal Medical Centre, Owerri, Imo State. As at 2012, five years prevalence of all cancer in Nigeria is 225,000 (53.1%).11 In all, 681 women were enrolled into the study. There were 347 breast cancer cases diagnosed and 344 controls managed in the health facilities were enrolled in the study. Purposive sampling method was used to select tertiary health institutions and a referral center for breast cancer in Imo and Abia States. All statistical analysis were performed using Statistical Package for Social Sciences (SPSS) version 23 software package13 Quantitative data were expressed as numbers and percentages while qualitative standards were expressed as Mean± Standard Deviation(SD). Independent T-Test was used to assess statistical differences in height, weight and BMI in studied group. Based on the BMI, women were grouped into four categories in which the odds ratio were calculated to find risk estimation between the group of BMI in both pre and postmenopausal women separately. Multiple logistic regression analysis was conducted to estimate the odds ratio for developing breast cancer and 95% confidence interval for variables. The second BMI category was used as a reference category. Less than 0.05 was regarded as significant statistical level.
Ethical Approval
The study received ethical approval from the Department of Public Health, Federal University of Technology Owerri, Abia State University Teaching Hospital, Aba, The Maranatha Specialist Hospital, Aba, and the Federal Medical Center, Owerri. Written informed consent was sought and obtained from each subject. Participation was voluntary and the study did not involve invasive procedures or the alteration of standard clinical care.
Results
Table 1 shows the frequency distribution for BMI for the total population and for pre- and post-menopausal women. Of the 681(100%) subjects studied, 345(50.7) were cases and 336(49.3%) were controls. The overall mean height and weight difference were 161.39 ± 6.6 and 65.9 ± 10.6, respectively. The subjects' BMI for underweight, normal, overweight and obese for cases were 17(5.0), 162(46.9), 99(28.7) and 67(19.4), respectively. The subjects' BMI for underweight, normal, overweight and obese for controls were 16(4.8), 152(45.2), 131(39.0), 37(11.0), respectively.
| Measurement | Frequency (%) | Mean | STD | Cases (%) | Controls (%) |
|---|---|---|---|---|---|
| Height | 681 (100) | 161.39 | 6.6 | 345 (50.7) | 336 (49.3) |
| Weight | 681 (100) | 65.9 | 10.6 | 345 (50.7) | 336 (49.3) |
| BMI | |||||
| Underweight | 33 (4.8) | 17 (5.0) | 16 (4.8) | ||
| Normal | 314 (46.1) | 162 (46.9) | 152 (45.2) | ||
| Overweight | 230 (33.8) | 99 (28.7) | 131 (39.0) | ||
| Obese | 104 (15.3) | 67 (19.4) | 37 (11.0) | ||
| Total | 681 (100) | 25.4 | 4.4 | 345 (50.7) | 336 (49.3) |
| Premenopausal | |||||
| Underweight | 14 (5.6) | 8 (6.2) | 6 (5.1) | ||
| Normal | 114 (46.0) | 61 (46.9) | 53 (44.9) | ||
| Overweight | 78 (31.5) | 33 (25.4) | 45 (38.1) | ||
| Obese | 42 (16.9) | 28 (21.5) | 14 (11.9) | ||
| Total | 248 (100) | 2.6 | 0.82 | 130 (100) | 118 (110) |
| Postmenopausal | |||||
| Underweight | 19 (4.4) | 9 (4.2) | 10 (4.6) | ||
| Normal | 200 (46.2) | 101 (47) | 99 (45.4) | ||
| Overweight | 152 (35.1) | 66 (30.7) | 86 (39.4) | ||
| Obese | 62 (14.3) | 39 (18.1) | 23 (10.6) | ||
| Total | 433 (100) | 2.6 | 0.79 | 215 (100) | 218 (100) |
Difference in Height, Weight and BMI
Table 2 presents the differences in height, weight and BMI between cases and controls for premenopausal and postmenopausal women. The premenopausal mean height for cases was 159.9± 8.0 compared to controls 161.7±5.6 (p<0.009); weight was 65.6±I3.0 compared to controls 65.7±9. 1 (p<0.0001); and BMI was 25.7±5.3 compared to controls 25.2± 3.8 (p<0.0001). When the mean height difference between cases and controls subjects were evaluated, a significant difference was observed indicating that the mean height was higher for pre-menopausal controls compared to cases and lower for postmenopausal controls compared to cases with (p<009).
| Measurement | Cases (Mean) ± SD | Controls (Mean)± SD | P -value | T-test | |
|---|---|---|---|---|---|
| Premenopausal Height | 159.9±8.0 | 161.7±5.6 | 0.009 | 2.066 | |
| Weight | 65.6±13.0 | 65.7±9.1 | 0.000 | 0.139 | |
| BMI | 25.7±5.3 | 25.2±3.8 | 0.000 | 0.891 | |
| Postmenopausal Height | 161.9±6.4 | 161.6±6.2 | 0.430 | ||
| Weight | 66.8±10.9 | 65.3±9.4 | 1.560 | ||
| BMI | 25.6±4.5 | 25.1±4.1 | 1.170 | ||
| BMI Total Height | 161.1±7.1 | 161.6±6.0 | <0.470 | 1.000 | |
| Weight | 66.3±11.8 | 65.4±9.3 | <0.000 | 1.100 | |
| BMI | 25.6±4.8 | 25.1±4.0 | <0.001 | 1.600 | |
Association between Breast Cancer Risks and BMI
Table 3 shows the association between breast cancer risk and BMI. There was a positive association between BMI and breast cancer risk and the risk is stronger for postmenopausal subjects compared to premenopausal subjects. The odds of developing breast cancer for women in the premenopausal category were 1.74, 1.50, and 2.21 higher for underweight, overweight and obese, respectively compared to controls, while the odds of developing breast cancer for women in the postmenopausal category were 1.66 and 2.72 higher for underweight and obese women compared to controls (Figure 1).
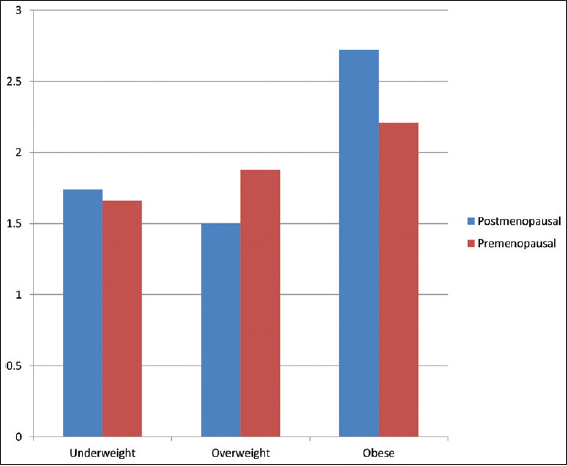
- Distribution of Odds Ratios and BMI categories in pre- and postmenopausal breast cancer risk among women
| Measurement | N (%) | Cases (%) | Control (%) | Odds ratio | p-value | 95% CI |
|---|---|---|---|---|---|---|
| Premenopausal | ||||||
| Normal | 114 (46.0) | 61 (46.9) | 53 (44.9) | 1-ref | 0.034 | |
| Underweight | 14 (5.6) | 8 (6.2) | 6 (5.1) | 1.740 | 0.143 | 0.829-3.641 |
| Overweight | 78 (31.5) | 33 (25.4) | 45 (38.1) | 1.500 | 0.521 | 0.435-5.172 |
| Obese | 42 (16.9) | 28 (21.5) | 14 (11.9) | 2.210 | 0.120 | 1.246-5.970 |
| Total | 248 (100) | 130 (100) | 118 (100) | |||
| Postmenopausal | ||||||
| Normal | 200 (46.2) | 101 (47.0) | 99 (45.4) | 1-ref | 0.045 | |
| Underweight | 19 (4.4) | 9 (4.2) | 10 (4.6) | 1.660 | 0.089 | 0.930-2.980 |
| Overweight | 152 (35.1) | 66 (30.7) | 86 (39.4) | 1.880 | 0.231 | 0.668-5.317 |
| Obese | 62 (14.3 | 39 (18.1) | 23 (10.6) | 2.720 | 0.010 | 1.204-4.054 |
| Total | 433 (100) | 215 (100) | 218 (100) | |||
| BMI Total | ||||||
| Normal | 314 (46.1) | 162 (46.9) | 152 (45.2) | 1-ref | 0.004 | |
| Underweight | 33 (4.8) | 17 (5.0) | 16 (4.8) | 1.700 | 0.023 | 1.070-2.690 |
| Overweight | 230 (33.8) | 99 (28.7) | 131 (39.0) | 1.700 | 0.187 | 0.772-3.763 |
| Obese | 104 (15.3) | 67 (19.4) | 37 (11.0) | 2.396 | 0.000 | 1.480-3.868 |
| Total | 681 (100) | 345 (100) | 336 (100) | |||
BMI categories in pre- and postmenopausal breast cancer risk among women
There was a total of 347 cases and 336 controls overall, in both pre-and postmenopausal women. Breast cancer risk was increased by increasing BMI, but the risk was more pronounced among postmenopausal than premenopausal women, especially for women with BMI more than 30 kg/m2. The results of multiple logistic regression show that a high BMI (more than 30 kg/m2) was positively correlated with risk of breast cancer development in both pre- and postmenopausal Nigeria women.
Discussion
There was a significant difference between the heights of patients with breast cancer for all women collectively with controls, which shows that breast cancer risk is associated with increased height. This is in agreement with the findings of other studies in Europe and Africa in which breast cancer risk was associated with increasing height in both pre- and postmenopausal women4,14,15 The increase in breast cancer risk seem to be associated with increase in height as expressed by Zhang et al.15 which showed that adult height is a risk factor for breast cancer in women and 10 cm increase in height was associated with a 17% elevated risk of breast cancer. The association between height and breast cancer risk may likely be due to a more complex interaction between genetic and environmental factors.4,15
Postmenopausal women obesity was a risk factor for developing breast cancer.16,17 As reported previously8,14,16,17 this study found that there was a statistically significant difference between the weight of controls [65.4±9.3, <0.01, CI=95%] and cases. [66.3±11.8 <0.01 CI= 95%]. This study also showed statistically significant differences in BMI between cases [25.6±4.8, p<0.001] and control [25.1 ±4.0, p<0.001]. The result is consistent with the results of studies by Dukyoo, et al.18 and Zhu et al.19
In this study, BMI were categorized into four (4) categories according to WHO classification namely: underweight (BMI< I8.5kg/m2); normal range (18.5 - 24.9kg/m2); overweight (25- 30kg/m2); and obese (BMI≥ 30kg/m2). The odds of developing breast cancer was 2.72 higher for postmenopausal obese women compared to obese women (OR=2.39) when Pre- and post menopausal women were combined (Figure 1).
Findings from this study show that as BMI increases, the risk of breast cancer in postmenopausal women increases. Our results are consistent with work done by Iwasaki et al.,14 Dukyoo et al.,18 Rosilene.et al.,20 and Cold et al.9 After menopause, being obese increases breast cancer risk. Women who were overweight or obese after menopause have a 30-60 percent higher breast cancer risk than those who were lean.16-17,21 Some studies have shown that fat tissue contains an enzyme called aromatase which converts hormones called androgens to estrogen which make women with higher BMI to have higher blood estrogen levels than leaner women22 which increases the chances of such women developing breast cancer compared to leaner women with lower estrogen levels. This explains some of the risk among postmenopausal women who were overweight.
The high risk of breast cancer associated with high BMI in postmenopausal women category in this study may also be attributed to high levels of insulin in their body. Women with high BMI tend to have higher levels of insulin compared to leaner women.23 Some studies24-26 have reported an association with an increased risk of breast cancer among postmenopausal women with high levels of insulin.
Limitations
The study examined the breast cancer risk in relation to BMI for premenopausal and postmenopausal Igbo women in two South East Nigeria states. Our results cannot be generalized to all women in Nigeria. The relationship between breast cancer and obesity was related to high estrogen levels in postmenopausal women, however, our study did not explore staging of breast cancer, or treatment modality in breast cancer as this was beyond the scope of the study.
Recommendations
Primary prevention measures such as increasing physical activity is important to modestly curtail the increasing burden of breast cancer. Other primary prevention methods include avoidance of greater BMI/obesity and avoidance of postmenopausal weight gain. More research on hormone replacement therapy (HRT) is recommended given that HRT increases the risk of breast cancer and there might be a possibility that menopausal women were on HRT.
Conclusion and Implications for Translation
Among the population, height, weight, and body mass index were associated with increased breast cancer risk. There was a positive association between BMI and breast cancer risk for both pre- and postmenopausal women, but the association was stronger among postmenopausal women.
Compliance with Ethical Standards
Conflicts of interest:
The authors declare that they have no conflict of interest.
Financial Disclosure:
None.
Ethics Approval:
Ethical clearance was obtained from the Ethical Committiee at Abia State University Teaching Hospital, the Maranatha Specialist Hospital, and Federal University of Technology, Owerri, Imo State, Nigeria.
Acknowledgements:
The study team appreciates the support of the Doctors and the participants for their cooperation during the study.
Funding/Support:
None.
References
- Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int. J. Cancer. 2013;132(5):1133-1145.
- [Google Scholar]
- Weight of communities: A multilevel analysis of body mass index in 32,814 neighborhoods in 57 low to middle- income countries (LMICs) Social Science and Medicine. 2012;75(2):311-22.
- [Google Scholar]
- Nigerian Demographic Profile. (accessed )
- Obesity and Height in urban Nigerian women with breast cancer. Ann Epidemiol. 2003;3:455-461.
- [Google Scholar]
- Case- control study of body size and breast cancer risk in Nigerian women. Am. J. Epidemiol. 2010;172(6):682-690.
- [Google Scholar]
- Body fat distribution and breast cancer risk: Findings from the Nigerian breast Cancer Study. Cancer Causes Control. 2012;23(4):565-574.
- [Google Scholar]
- Relationship of body mass index with aromatization and plasma and tissue oestrogen levels in postmenopausal breast cancer patients treated with aromatase inhibitors. European Journal of Cancer. 2014;50:1055-1064.
- [Google Scholar]
- Obesity is associated with a poorer prognosis in women with hormone receptor positive breast cancer. Maturitas. 2014;79(3):279-286.
- [Google Scholar]
- A woman's build and the Risk of Breast Cancer. European Journal of Cancer. 1998;34:1163-1174.
- [Google Scholar]
- Body fatness at young ages and risk of breast cancer throughout life. American Journal of Epidemiology. 2010;171:1183-1194.
- [Google Scholar]
- 2013. GLOBOCAN 2012 v 1.0 cancer incidence and mortality worldwide.
- Decline in invasive breast cancer and use of post menopausal hormone therapy in a screening mammography population. J Nat Cancer Inst. 2007;99(17):1335-9.
- [Google Scholar]
- Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp;
- [Google Scholar]
- Body size and Risk for Breast cancer in Relation to Estrogen and Progesterone Receptor Status in Japan. Ann Epidermiol. 2007;17(4):304-3112.
- [Google Scholar]
- Height and breast cancer risk: evidence from prospective studies and mendelian randomization. J Natl Cancer Inst. 2015;107(11):djv219.
- [CrossRef] [Google Scholar]
- Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ. 2007;335(7630):II34.
- [Google Scholar]
- BMI and Breast cancer in Korean Women: A meta- Analysis. Asian Nursing Research. 2009;3(1):31-40.
- [Google Scholar]
- Payne-Wilks K, Texter L. Body mass index and breast cancer risk in African American women. Ann Epidemiol. 2005;5:123-128.
- [Google Scholar]
- Relationship between body mass index, waist circumference and waist to hip ratio and the steroid hormone receptor status in breast carcinoma of pre- and postmenopausal women. The Breast. 2009;8:8-12.
- [Google Scholar]
- Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am J Epidemiol. 2000;152:514-27.
- [Google Scholar]
- for the Endogenous Hormones and Breast Cancer Collaborative Group. Circulating sex hormones and breast cancer risk factors in postmenopausal women: reanalysis of 13 studies. Br J. Cancer. 2011;105(5):709-22.
- [Google Scholar]
- Quantifying mediating effects of endogenous estrogen and insulin in the relation between obesity, alcohol consumption, and breast cancer. Cancer Epidemiol Biomarkers Prev. 2012;21(7):1203-12.
- [Google Scholar]
- for the Nurses' Health Study. Type 2 diabetes and subsequent incidence of breast cancer in the Nurses' Health Study. Diabetes Care. 2003;26(6):1752-8.
- [Google Scholar]
- Diabetes and breast cancer risk: a meta-analysis. Br J Cancer. 2012;107(9):1608-17.
- [Google Scholar]
- Systematic review and meta-analysis of the association between diabetes mellitus and incidence and mortality in breast and colorectal cancer. Br J Surg. 2013;100(11):1421-9.
- [Google Scholar]





