Translate this page into:
Gestational Diabetes Mellitus and Associated Health Risk Outcomes in Mothers and Neonates
✉Corresponding author email: lornaloo.adoyo@gmail.com
-
Received: ,
Accepted: ,
Abstract
Globally, Gestational Diabetes Mellitus (GDM) pregnancy complication is estimated at 200,000 cases annually with serious consequences for maternal and neonatal health. A cohort study to establish GDM risks and associated health outcomes was conducted among 238 women attending an antenatal clinic in selected health facilities in Nairobi, Kenya. Results indicated that mothers with GDM are four times more likely to have varied physical discomforts and complicated deliveries as a result of high neonatal birth weight. There is a need to advocate for the inclusion of diabetes testing and management as part of Kenya's Essential Health Services Package to realize positive health outcomes among women.
Keywords
Gestational Diabetes Mellitus
Maternal
Neonates
1. Introduction
Gestational Diabetes Mellitus (GDM), defined as any degree of glucose intolerance with onset or first recognition during pregnancy, is one of the health conditions that has been neglected until a decade ago, when there was a notable increase of non- communicable disease cases globally. The prevalence of GDM is estimated to be in the range of 1 to 14% of all pregnancies, depending on the population characteristics being studied and the diagnostic technique.1 Globally, GDM Pregnancy complications are estimated at 200,000 annually.2 Further, the outcome of GDM in population is of greater magnitude touching on maternal GDM also adversely impacts neonatal health. Mothers suffer the physical discomfort associated with type 2 diabetes, while for their offspring the risks may include fetal macrosomia, hypoglycemia, jaundice, polycythaemia, obesity and diabetes in late adolescence or young adulthood.
Perinatal mortality risks associated with GDM are mostly attributable to undiagnosed type 2 diabetes, which is common among mothers with obesity. Other complications, such as congenital malformation in neonates, are slightly increased in infants of mothers with GDM (whether untreated, moderate or severe) as compared to the general population. It is worth noting that GDM prevalence has increased by approximately 10-100% in the last 20 years.3 This is a reflection of the patterns of increasing diabetes and obesity conditions in the population. A systematic review from 2014 also indicated that little is known about GDM in Africa and highlights the need for further research.3
Kenya continues to report worrying statistics in Non-Communicable Diseases (NCDs), diabetes included. The prevalence of such diseases in the younger population underscores the need for an investigation to be conducted to identify predisposing factors that need modifications in order to realize improvements in health outcomes for mothers and neonates. The sudden upsurge of diabetes among Kenya's young population is estimated at about 1.8 million people living with diabetic condition.4 The soaring numbers and the youngest diagnosed infant case in Kenya have amplified the need for action. Reviewed studies also indicate that there is a likelihood that future generations have chances of developing obesity and other non-communicable health problems that are mostly determined in the womb, hence the interest in studying gestational diabetes and the associated health risks.5 Evidence-based information on gestational diabetes and associated perinatal health risks will likely increase acceptability of research findings. That acceptance will go a long way in informing the general public on issues related to nutrition and lifestyle during pregnancy and after child birth, giving rise to desirable health outcomes among mothers and neonates. The objective of this study was to examine risks and health outcomes among mothers with GDM compared to non-GDM mothers.
2. Methods
This cohort study was conducted to evaluate risks and possible outcomes in GDM condition among pregnant women. Nairobi County was considered as the study site on the basis of being a populous city, with population estimate of 3 million people,6 and having desirable characteristics in relation to urbanization and sedentary lifestyle, key drivers to the evolution of NCD epidemics in developing countries.
2.1. Study Population, Sample Size and Inclusion Criteria
The study population was comprised of women in their third trimester of pregnancy, and sample size was determined for the two groups (GDM and non-GDM) with 10% effect size at 95% confidence Interval (CI). The existing high birth weight among the GDM group was estimated at 13% and 23% among non-GDM group. To factor in potential attrition, the obtained sample of 231 participants was then increased by 10% to 254 for mother-baby pair. Simple random sampling technique was used to select 10 facilities from the Master Facility List (MFL).
2.2. Study Procedure and Data Collection
Oral Glucose Test (OGT) was conducted to ascertain GDM condition and also for categorization into GDM and non-GDM groups necessary for making comparison. Participants were required to continue with normal diet one hour leading up to the test, while avoiding bathroom visits before the procedure. After blood sample collection, participants were instructed to have a sweet drink or concentrated glucose solution. Within five minutes after which glucose levels were tested again. Structured questionnaires were also administered in three phases to assess initial eligibility, record prevailing physical condition during pregnancy, and a follow up interview within 28 days after giving birth. Figure 1 shows the methodological diagram of the study.
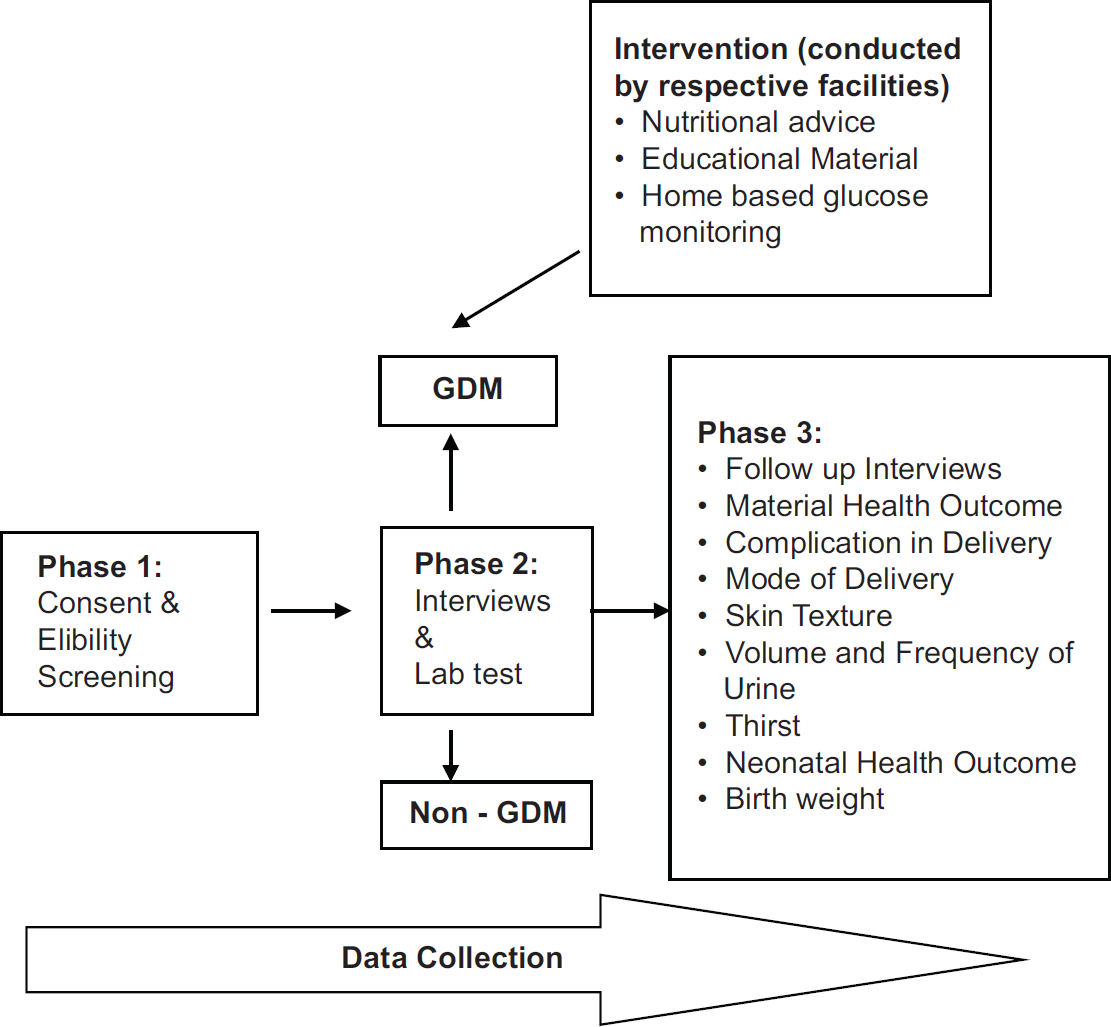
- Methodological diagram
2.3. Statistical Analysis
Using Stata version 13,7 risk factors were analysed as odds ratio and univariate logistic regression analysis was conducted for nominal, ordinal and interval variables such as BMI, age, and birth weight, respectively. Multilevel logistic regression was applied to account for confounding variables by analysing GDM and non- GDM independent variables in order to predict health outcomes in mothers and neonates.
2.4. Ethical Approval
Ethical Review Committee of Kenyatta National Hospital in conjunction with the University of Nairobi verified the conformation of research to ethical requirements in handling human subjects. Written permission was obtained from both local authorities and management of the selected maternity facilities. Additionally, study participants were required to consent to participate in the study. Confidentiality was maintained by assigning participants unique codes and resulting information was used only for study purposes and recommendations towards Maternal and Child Health Intervention Programs, including policy changes that were intended for the benefit of the population in Kenya and the region. Investigators engaged in the study underwent certification process by ethically certified scientific body - CITI, and all ethical practices were adhered to.8
3. Results
Overall, the study had 238 participants who completed the follow-up process; of these responses 66 mothers [27.73%] had GDM. The analysis of trend showed that mothers with family history of diabetes had twice the risk of developing GDM [OR= 2.27; 95% CI: 1.23-4.17], in comparison with mothers who did not have family history of diabetes. Additionally, body mass index (BMI) showed a positive association with GDM, with findings indicating that obese mothers had doublefold increased risk of developing GDM [OR= 28; 95% CI: 11.83-36.7]. Similarly, age showed a positive association with GDM condition in mothers [OR = 1.15; 95 % 0:1.089-1.206].
In relation to physical discomfort, results indicated that mothers with GDM were four times more likely to experience high frequency of urination [OR = 4.33; 95% CI: 1.14-16.47], produced three times higher volume of urine [OR = 3.65; 95% CI: 1.12-11.93], while episiotomy mode of delivery [OR=0.29; 95% CI:0.10-0.85] and skin texture [OR=0.17; 95% CI:0.077- 0.385] showed negative association, but remained significantly common among GDM mothers [p-value <0.05]. Similarly, high blood pressure was more common among GDM mothers, 23 [38.89%] compared to 27 [18.75%] non-GDM mothers.
Neonatal birth weight was nine times higher among GDM mothers [OR = 9.69; 95% CI: 0.01 - 0.59]. Consequently, the association of GDM and high neonatal birth weight was also highly significant [p- value=0.0l 3]. Cesarean Section (CS) mode of delivery was high: 38 [58.46%] among mothers with GDM compared to 60 [35.55%] for mothers with non-GDM condition. Table 1 shows demographic characteristics of participants and associated health outcomes in GDM and non-GDM group.
| Indicator | GDM (n=66) % | Non-GDM (n=172) % | OR (95 CI) | p-value |
|---|---|---|---|---|
| Diabetic History | ||||
| No diabetic history (Ref.) | 62.3 | 42.11 | 1.00 | |
| Had diabetic history | 37.7 | 57.89 | 2.27 (1.23, 4.17) | 0.008 |
| BMI before pregnancy | ||||
| Underweight (Ref.) | 1.5 | 7.74 | 1.00 | |
| Normal | 19.70 | 56.55 | 1.78 (0.214, 14.74) | 0.593 |
| Overweight | 54.55 | 35.12 | 7.93 (0.99, 63.22) | 0.051 |
| Obese | 24.24 | 0.06 | 2.08 (1.83, 3.65) | 0.000 |
| Extreme obese | 0.0 | 0 | ||
| Mean age | (31.59,34.32) | (27.01,28.78) | 1.15 (1.089, 1.206) | 0.000 |
| Urine frequency per day | ||||
| <= 2 hours (Ref.) | 12.31 | 18.35 | 1.00 | |
| 3-4 hours | 53.85 | 70.25 | 0.99 (053, 1.87) | 0.983 |
| >= 4 hours | 33.85 | 11.39 | 1.90 (0.81,4.46) | 0.141 |
| Volume of urine per day | ||||
| Little (Ref.) | 21.54 | 39.75 | 1.00 | |
| Normal | 52.31 | 46.58 | 2.07 (1.02, 4.19) | 0.043 |
| A lot | 26.15 | 13.66 | 3.53 (1.50, 8.33) | 0.004 |
| Skin texture | ||||
| Soft and glowing (Ref.) | 24.62 | 47.17 | 1.00 | |
| Dry and rough | 75.38 | 52.83 | 0.37 (0.19, 0.69) | 0.002 |
| Blood pressure | ||||
| Normal (Ref.) | 61.67 | 18.35 | 1.00 | |
| High | 38.33 | 70.25 | 2.53 (1.29, 4.94) | 0.007 |
| Low | 0.0 | 11.29 | ||
| Neonates birth weight | ||||
| Underweight <2.5Kg (Ref.) | 1.52 | 7.65 | 1.00 | |
| Small 2.6Kg-3.5Kg | 31.82 | 57.65 | 2.78 (0.35, 22.47) | 0.336 |
| High birth weight | 66.67 | 34.71 | 9.69 (0.01, 0.59) | 0.013 |
4. Discussion
The probability of GDM mothers developing type 2 diabetes after birth was highly significant, hence the findings rejected the null hypothesis that there is no difference in maternal health outcome between women with GDM and those without GDM. Symptoms related to diabetic condition in GDM mothers, such as feeling thirsty, high frequency of urination and a large volume of urine, was significantly expressed during pregnancy and persistent after delivery. These study results are consistent with a study done by Ferrara and the American Diabetes Association indicating that frequency of GDM usually reflects the frequency of type 2 diabetes in the underlying population, with more than 50% developing type 2 diabetes within 5-10 years after delivery.9
High neonatal birth weight was found to be positively associated with GDM condition in mothers, with estimated cases to be 44 [66.67%] compared to neonates delivered by non-GDM mothers 59 [34.71%]. High birth weight phenomena, also referred to as macrosomia, was observed in another report which showed a positive correlation between maternal blood glucose levels and increased birth weight.9 Findings in other studies also give indication that women with GDM are more likely to give birth to macrosomia or large-for-gestational-age infants resulting to complications such as obstructed labor, a birth injury for the infants and the death of the mother or the baby or both.
4.1. Limitations
A much larger sample size given the high birth rate in the country would have been more desirable for any robust cohort study. However, due to limitations in time and material resources, the study was restricted to 6 sub-Counties of Nairobi with a total of 10 facilities out of the 97 selected for the study. This also meant that it took a long time to achieve minimum desirable and statistically adequate sample.
Loss-to follow up was evident when mothers failed to enrol Post-Natal Care (PNC), either because they sought for well-baby clinic services elsewhere outside selected study facilities or other unknown reasons as they could not be traced via telephone nor to their residences. To make the study finding generalizable at acceptable levels, attrition was catered for by increasing sample size by 10%.
Study had standardization limitations in OGT as the study relied on different laboratories where participants chose to conduct their tests. It is possible that the different settings might have affected precision of the tests. Thus, the researchers recommend the inclusion of screening resources in the future to improve accuracy in test results and effectiveness of the research process. In order to establish true prevalence and the impact of GDM, there is a need to conduct a study with robust methodological approach using standardized and optimal diagnosis procedures for GDM and recruitment of adequate sample size with a longer follow up period of between 2-5 years after delivery.
5. Conclusion and Implications for Translation
Elevated blood glucose in pregnant mothers, also known as GDM, is a precursor to complications during pregnancy and may result in obstructed labor leading to cesarean section birth due to increased chances of having large gestational weight in neonates.
Compliance with Ethical Standards
Conflicts of Interest:
The authors declare that they have no conflict of interest.
Financial Disclosure:
This study was solely funded by individual resources.
Funding/Support:
None.
Ethics Approval:
Ethical review was given by Scientific Commitee of Kenyatta National Hospital/Unversity of Nairobi and relevant approvals were issued.
Disclaimer:
None.
Acknowledgments:
The authors thank the management of health facilities and participants. Dr. Adoyo acknowledges the professionalism of Ethics Committee and thanks her mentors, Dr. Yeri Kombe and Professor Charles Mbakaya. Special tribute to Prof. Venny Nyambati who succumbed to cancer just before the completion of the study project.
References
- Society for Maternal-Fetal Medicine. 2010. High-Risk Pregnancy Care, Research, and Education for Over 35 Years. http://www.mfmnyc.com/wp-content/uploads/2015/10/SMFMMonograph3.1.pdf (accessed )
- [Google Scholar]
- Gestational Diabetes: What Patients Need to Know. Pharmacy Times. https://www.pharmacytimes.com/publications/issue/2009/october2009/CounselingGestationalDiabetes-1009. Published October 15, 2009 (accessed )
- [Google Scholar]
- Gestational diabetes mellitus in Africa: a systematic review. PLos One. 2014;9(6):e97871. 10.1371/journal.pone.0097871
- [CrossRef] [PubMed] [Google Scholar]
- A population-based survey of prevalence of diabetes and correlates in an urban slum community in Nairobi, Kenya. BMC Public Health. 2013;13(1):371. 10.1186/1471-2458-13-371
- [CrossRef] [PubMed] [Google Scholar]
- Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care. 2007;30(8):2070-2076. 10.2337/dc06-2559a
- [CrossRef] [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics (KNBS) 2010. The 2009 Kenya Population and Housing Census - Population Distribution by Age, Sex and Administrative Units. 1C:546. http://www.knbs.or.ke/index.php?option=com_phocadownload&view=category&download=584:volume-1c-population-distribution-by-age-sex-and-administrative-units&id=109:population-and-housing-census-2009&Itemid=599 (accessed )
- [Google Scholar]
- CITI Program: Collaborative Institutional Training Initiative. https://www.citiprogram.org (accessed )
- [Google Scholar]
- Pregnancy complications and maternal cardiovascular risk: opportunities for intervention and screening? BMJ. 2002;325(7356):157-160. 10.1136/bmj.325.7356.157
- [CrossRef] [PubMed] [Google Scholar]





