Translate this page into:
Impact of COVID-19 on Essential Health Care of Rural People in Northern Bangladesh: A Cross-Sectional Study
✉Corresponding author email: dr_matiur@yahoo.com
Abstract
Background and Objectives:
The coronavirus disease 2019 (COVID-19) has an unpredicted effect on global society. The main objective of this study is to determine the impact of COVID-19 on rural people's access to health care in Northern Bangladesh.
Methods:
A cross-sectional community-based design was used. Data were collected from four different districts in the Rajshahi and Rangpur divisions using the multistage sampling technique. A pre-tested semi-structured questionnaire was used for data collection. SPSS version 25 was used for the statistical analysis.
Results:
Among 639 respondents, 59.5% were female, and 40.5% were male. The mean age was 34.3 years (SD ±10). The family income ceiling was reduced to -15.6% for incomes between $10,000 and $20,000, and -12.7% for incomes between $20,000 and $30,000. Because 38.2% of respondents' income was reduced during COVID-19, they now fall into the income category of ≤10,000 Bangladeshi Taka. Due to a lack of transportation, 41.7% of respondents never sought medical attention. During the COVID-19 period, respondents reported physical illness (24.4%), severe stress problems/mental illness (39.2%), and either injuries or urgent health problems (3.8%). The percentage of respondents who did not seek medical attention because they were afraid of becoming infected with COVID-19 was 30.3%. The majority of respondents, 67.3% (n=188), stated that they were unable to locate any maternal and child health care institutions.
Conclusion and Implications for Translation:
The COVID-19 pandemic caused a significant disruption in the delivery of essential health services. To address future COVID-19 outbreaks and similar pandemics, the government and private sector must work together, as well as global collaboration.
Keywords
COVID-19
Access to Essential Health Care
Rural People of Bangladesh
Introduction
Background of the Study
The outbreak of novel coronavirus-2 (nCoV-2) was declared a global pandemic and an international public health emergency by the World Health Organization (WHO). It is a rapidly evolving and emerging situation, and the entire world is working to address it. As of October 2, 2022, over 615 million confirmed cases, and over 6.5 million deaths had been reported globally.1 The estimated basic multiplication number of the virus is significantly higher than many other infectious diseases, and this can potentially result in the capacity of health facilities becoming overwhelmed, even in countries that have the most developed health care systems.2 Globally, an estimated case fatality rate was 0.27% to 10%,3 which is 20% in Bangladesh, with some sporadic cases of serious illness in younger individuals, adults >60 years of age, and with co-morbid conditions make up the most vulnerable group.4 Worldwide, billions of people were staying at home to minimize the transmission of the virus. Along with other countries, Bangladesh is adopting preventive measures, such as hand washing social distancing, remote office activities, and mandatory lockdowns.5
Bangladesh, a developing country with one of the world's most densely populated areas, has been struggling to combat the spread of the disease since March 2020.5 Since then, infections have spread exponentially, with the rate being highest in Asia with wider community-level transmission. To prevent the spread of this virus, there are numerous actions taken by the government, such as countrywide lockdowns, travel restrictions, hazard controls in the workplace, cancellations and postponements of events, border enclosure, and screening at airports.5 These kinds of preventive and control measures, such as lockdown, hindered the normal flow of raw materials, products, and services and capital, resulting in temporary business and production shutdowns.5 This pandemic has led to acute global socioeconomic disruption, resulting in extensive scarcity of supplies. People experience mental stress and financial instability as a result of ceasing daily activities.6 To prevent a coronavirus, outbreak the government of Bangladesh declared a 10-day general holiday, on March 22, effective from March 26, which was later extended five times May 30, 2020.7 As of July 31, 2020, the government of Bangladesh had tested 1,176,809 samples, with a total of 237,661 confirmed cases, nearly 135,136 recoveries, and more than 3,000 deaths in the country.8 Community transmission, countrywide lockdown, loss of livelihood, and fear of infection lead to the severe suffering in poor and vulnerable communities in both urban and rural areas.9 In Bangladesh, preventive and control measures have been found challenging to implement due to a lack of general awareness of COVID-19 and the absence of a social safety net.7
According to WHO, Bangladesh has a severe shortage of physicians, nurses, and medical personnel.10 The country has the second-lowest doctor-to-patient ratio in South Asia, with 5.26 per 10,000 inhabitants.10,11 These shortcomings have also been highlighted as a result of the COVID-19 outbreak. Furthermore, most hospitals suspended routine operations, leaving non-COVID-19 patients without access to regular check-ups, maternal and child health services,12 and treatment. Some hospitals were also hesitant to accept in-patients for fear of being exposed to the virus.12 To address this issue, in May 2020, the Ministry of Health and Family Welfare issued a circular requiring all public and private hospitals to render health care services to non-COVID-19 patients as well,12 which was made possible by amending the Communicable Diseases Act of 2018. The government added the life-threatening COVID-19 to the list of contagious disorders after a supreme court directive.12
According to the report of United Nations International Children's Emergency Fund (UNICEF) on May 7, 2020, pregnant mothers and babies born during the COVID-19 pandemic were threatened by strained and disrupted health services. With 116 million expected births in the approximately 9 months since the COVID pandemic was recognized, UNICEF urges governments and donors to maintain life-saving services for pregnant women and newborns.13 During the lockdown, due to the fear of community transmission, private hospitals and clinics stopped providing any services to the public.14,15 Consequently, with the shortage of health care facilities for primary and critical care, the treatment of patients was greatly affected.16 The health care workers who were attending to the patients became infected and faced social stigma and discrimination from local people.16,17 In many places, public protests were observed against establishing quarantine facilities in their neighborhood and preventing COVID-19 care hospitals and clinics from accepting COVID-19 cases for fear of catching the virus. Social humiliation was a common practice. Thus, law enforcement authorities and government officials took the necessary steps to resolve this issue.16 There were many instances in which family members abandoned the infected and deceased loved ones in hospitals.12 The deceased persons were not given decent burials in local graveyards, which are basic cultural rights of Muslims.18 Moreover, those earning daily wages and low- and middle-income people who lost their jobs due to the lockdowns were particularly hard hit. For example, Bogura, a district city of northern Bangladesh, experienced rapid transmission of the coronavirus, causing residents to encounter an unusual situation in which their normal livelihood was halted.
Evidence showed that earnings, transportation, treatment, movement, farming, business, and other income-generating activities (IGAs) had been postponed because of the declared strict lockdown and quarantine since March 2020.19 People were suffering in both urban and rural areas due to limited access to basic needs. The anxiety and fear of death from hunger or death from infection led to several suicidal cases.20,21 Considering the human COVID-19 situation, the Research, Planning, and Development Department of the Thengamara Mohila Sabuj Sangha (TMSS) Health Sector conducted a rapid study on the effect of COVID-19 on the livelihood and access to health care of the rural people of northern Bangladesh.
Objectives of the Study
This study was conducted to identify the impact of COVID-19 on access to essential health care services for the rural people of northern Bangladesh. The specific aims of the study were as follows: (1) to identify the selected socio-demographic profile of rural people in northern Bangladesh and (2) to identify the accessibility of rural people to health care during the COVID-19 pandemic.
Methods
Study Design and Setting
A cross-sectional community-based survey design was used to assess the impact of COVID-19 on the essential health care of rural people in northern Bangladesh, applying a quantitative approach. The study was conducted during the lockdown period of the first wave of the COVID pandemic in Bangladesh (May 2020 to August 2020). It was conducted in the randomly selected four administrative districts (Bogura, Gaibandha, Joypurhat, and Naogaon) out of 16 districts under Rajshahi and Rangpur divisions in northern Bangladesh.
Recruitment Procedure
A carefully selected sample of individuals was interviewed face to face to assess the impact of COVID-19 on essential health care. The inclusion criteria included Bangladeshi citizens with a minimum age of 18 years who are the beneficiaries of TMSS. To ensure the fulfillment of the inclusion criteria, we asked the respondents about their birth year and whether they had a national identity card (which is only available to Bangladeshis over the age of 18 years). Respondents who were physically and psychologically ill and refuse to participate were excluded from the study.
Sample Size Determination
Before data collection, we estimated the sample size for this study. We assumed that 50% (p=.05) of the population had access to health care services during the lockdown. With a 95% confidence level and a 5% precision level, a representative sample of 384 was estimated using this proportion. The sample size increased to 576 and 720 after adjusting for the 1.5 design effect and the 20% non-response rate. This study proposed 720 individuals who were eligible for this study from four districts (not in proportion; Bogura 31.6%, Gaibandha 26.3%, Naogaon 24.5%, and Joypurhat 17.6%) of whom 645 consented to participate and another 75 declined. A total of 639 completed interviews were used to analyze data after excluding incomplete interviews. Multistage sampling techniques were used in this study. After randomly selecting four districts out of 16, two Upazila (sub-districts) from each district were also selected randomly. Then, two union Parishad from each selected Upazila were taken following the same method. The data were collected from the 16 union Parishads.
Data Collection
A pre-tested and semi-structured questionnaire was used in the study. The data collection technique was a personal interview of the study subjects. During the personal interview, all the instructions and guidelines of the Bangladesh government and WHO related to COVID, particularly maintaining social distancing and implementing protective measures, were followed. Data collected were reviewed for completeness and consistency by the supervisors and the principal investigator on a daily basis. The individual survey questionnaire consisted of two sections. The first section focused on socio-demographic and economic characteristics, including age, gender, education, occupation, current residence, religion, marital status, number of household members, living conditions, and income level. The second section covered the questions related to the accessibility to health care during the lockdown (including the status of experiencing any health issue, access to the health care institution and, the cause of low accessibility). To maintain the quality of the data, the data collection tools were adapted from standard questionnaires and carefully designed based on the objectives of the research. The questionnaire was reviewed by two sectoral experts, piloted on 20 adults, and finalized to ensure that the respondents understood all questions.
Statistical Analysis
Data were input, cleaned, and analyzed using SPSS version 25 software (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0., IBM Corp., Armonk New York). Percentages frequencies, charts, and cross-tabulations were used to describe the major characteristics of respondents.
Ethical Approval
The research protocol, questionnaire, consent statement, and procedures for obtaining informed consent were approved by the Ethical Review Committee (2020/01) of the TMSS Medical College, Bogura, Bangladesh. At the beginning of the interviews, written consent was taken from the respondents after conveying that full confidentiality of personal data would be strictly maintained. The purpose of the study was also explained to each of the participants, and they were informed about their rights to voluntarily join and withdraw from the interview at any point before the survey. Face-to-face interviews were conducted by maintaining social distancing and taking protective measures. Primary treatment was available in case of any emergency; the data enumerator is instructed to immediately communicate with the researcher or to the nearest health care facilities in case a respondent(s) needed medical assistance.
Results
Socio-Demographic Characteristics
According to the data gathered it has been shown that among the total of 639 respondents, 59.5% were female and 40.5% were male. The age group 21-30 years was represented by 37.7% of respondents followed by the age group 31-40 years (34.9%). It is clear that only the lowest percentage of respondents (1.6%) were older than 60. The mean age of the respondents was 34.3 years with an SD ±10 years. Of the total respondents, 92% were Muslim, and the rest were Hindu and other religions.
Educational qualification is another variable that has been used to know people's psychological construction, survival strategy, and social status. In terms of the level of education, the highest, (26.8%), had completed primary education, followed by the completion of a Junior School Certificate (JSC), Secondary School Certificate (SSC), and Higher Secondary Certificate (HSC) of the respondents, which were 21.4%, 17.7%, and 10.5%, respectively. The percentage of respondents who had completed a master's and above master's degree was found to be 4.4% and 0.2%, respectively. Married respondents were highest at 89.8%, whereas both divorced and separated were lowest (5% each). The majority of the respondents identified as being a housewife (46.3%), followed by those service holders (21.4%). The rest of the sectors were day laborers, students, farmers, physicians, and business owners, which were 3.1%, 5.2%, 6.7%, 8%, and 11.9%, respectively (Table 1).
| Characteristics | Frequency | % |
|---|---|---|
| Sex | ||
| Male | 259 | 40.5 |
| Female | 380 | 59.5 |
| Educational Qualification | ||
| Illiterate | 62 | 9.7 |
| Primary | 171 | 26.8 |
| Junior School Certificate | 137 | 21.4 |
| Secondary School Certificate | 113 | 17.7 |
| Higher Secondary Certificate | 67 | 10.5 |
| Honors | 60 | 9.4 |
| Masters and above | 29 | 4.6 |
| Occupational Status of the Respondents | ||
| Service Holder | 137 | 21.4 |
| Physician/Nurse/Health Worker | 05 | 0.8 |
| Business Owner | 76 | 11.9 |
| Farmer | 43 | 06.7 |
| Day Laborer | 20 | 3.1 |
| Unemployed | 15 | 2.3 |
| Housewife | 296 | 46.3 |
| Student | 33 | 5.2 |
| Others | 14 | 2.2 |
| Family Head | ||
| Male | 575 | 90.0 |
| Female | 64 | 10.0 |
| Household Size | ||
| Small Family (1-3 Members) | 196 | 30.7 |
| Medium Family (4-6 Members) | 396 | 62.0 |
| Large Family (≥7 Members) | 47 | 7.4 |
| Children under 5 Years | ||
| Yes | 248 | 38.8 |
| No | 391 | 61.2 |
Among all respondents, 80.1% were from the “nuclear family” and 19.9% from the “joint family.” Regarding household heads, 90% were headed by males, and 10% were headed by female members of the family. The household size of the respondents was categorized into three types: small, medium, and large family. A family of four to six members, called a medium family, represented 62%, whereas a large family consisting of seven or more members represented 7.4%. However, it was found that 30.6% are small families with one to three members, and 61.2% of respondents had no children aged under 5 years old, but the rest of 38.8% informed that “they had children aged 5 years and older.” The same consideration was initiated for knowing the number of the families with adult members living in households (HHs) of the respondents. Of the respondents, 79% said that they had no adult family members, whereas 21% had adult family members more than 60 years old. According to the data obtained, 97.5% of respondents' families do not have disabled members, but only 2.5% of respondents' families had disabled family members.
Main Variables (Dependent or Outcome) Result
According to the data collected, 432 respondents (67.6%) said that their households faced health problems during the COVID-19 pandemic. Five categories of health problems were identified by the respondents. Among them were physical illness (24.4%), severe stress problems (33.1%), either injuries or urgent health problems (3.80%), mental illness (6.30%), and respondents who faced no health-related problems (32.40%).
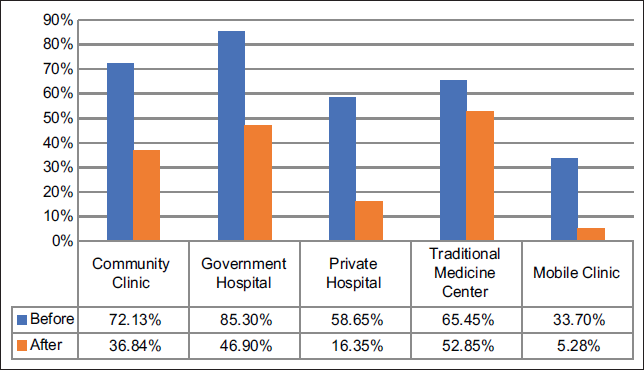
Multiple responses regarding the accessibility of health institutions before and during the onset of COVID-19 revealed that respondents received services from community clinics (36.84%), government hospitals (46.90%), private hospitals (16.35%), traditional medicine centers (52.85%), and mobile clinics (5.28%). Prior to treatment, it was found that the highest percentage of the respondents (85.3%) relied on government hospitals and the lowest percentage of the respondents (33.7%) relied on community clinics. The reasons for the low access to health institutions during the novel coronavirus were that 41.7% of participants never used health facilities due to the unavailability of transportation to health institutions, which is marked as the highest, and only 7.4% of respondents had low access to health services due to unavailability of health institutions as lowest. However, it is known that another 30.3% (131 respondents) did not go to health institutions due to the fear of getting an infection from COVID-19. Finally it was found, that respondents always struggle to get access to health institutions during COVID-19 for taking treatment. During COVID-19, it was determined that 32.97% of respondents had accessed maternal and child health institution services. In contrast, 67.3% of them said that they could not find any health institutions for getting treatment and necessary services. The major reasons for failing to take the services for maternal and children were fear of getting infected by COVID-19 (37.4%) and due to unavailability of transportation to reach health institutions (30.8%). However, highly unconventional identification has been revealed, such as no doctors were present at health institutions (13.5%) and health institutions were not open (05.6%), which has a negative impact on the treatment and care of pregnant mothers and children (Table 2).
| Characteristics | Frequency | % |
|---|---|---|
| Status of experiencing any health issues during COVID-19 | ||
| Yes | 432 | 67.6 |
| No | 207 | 32.4 |
| Types of health issues experienced during the COVID-19 pandemic | ||
| Physical Illness | 156 | 24.4 |
| Severe Stress | 212 | 33.1 |
| Injury/Emergency | 24 | 3.8 |
| Mental Illness | 40 | 6.3 |
| No Problem | 207 | 32.4 |
| Reasons behind the low access to health institutions | ||
| Unavailability of transportation to reach Health Institutions | 180 | 41.7 |
| Health Institutions were not open | 32 | 07.4 |
| No doctors are present at Health Institutions | 48 | 11.1 |
| Health institutions were open but disagree to provide the service | 41 | 09.5 |
| Didn't go to health institutions because of fear of getting infected by COVID-19 | 131 | 30.3 |
| Access to maternal and child health institutions during the COVID period (n=188) | ||
| Couldn't access | 126 | 67.30 |
| Access | 62 | 32.97 |
| Reasons behind the low access to maternal and child health institutions | ||
| Unavailability of transportation to reach health institutions | 39 | 30.8 |
| Health institutions were not open | 07 | 05.6 |
| No doctors are present at health institutions | 17 | 13.5 |
| Health Institutions were open but refrained from providing the service | 16 | 12.7 |
| Didn't go to Health Institutions because of fear of getting infected by COVID-19 | 47 | 37.4 |
Figure 1 shows the rate of difficulty in getting maternal and child health services in respondents' households during COVID-19. According to the data it has been found that 70.60% faced problems in getting health services for their children, whereas 29.40% stated that they had no problems.
- Access to Health Institutions before and after the onset of COVID-19
Other Variable(s) (Covariates) Results
The monthly income of respondents' households before and during COVID-19 has seen an average decrease in the income ceiling. Respondents' HH income ceiling was reduced by -15.6% for those earning $10,001-20,000, and by -12.7% for those earning $20,001-30,000. Another concern is that 38.2% of respondents' income was reduced during COVID-19, and they now belong to the income group ≤10,000 BDT. Expenditure is determined by income, and it was identified that all types of income groups experienced a decrease in their earnings during COVID-19. As previously stated, 7.5% of respondents had monthly expenditures ranging from 10,000 to 15,000 BDT (Bangladeshi Taka), whereas the majority of the highest income categories had expenditures ranging from 15,001 to more than 30,000 BDT.
The average expenditure of the respondents also decreased from 15,598 to 11,458 before and during COVID-19, respectively, and the difference was almost 4,140 BDT on average for every respondent (Table 3).
| Income Source | Before COVID | During COVID | ||
|---|---|---|---|---|
| n | % | n | % | |
| Salary | 140 | 21.9 | 95 | 14.9 |
| Daily/Casual Laborer | 122 | 19.1 | 101 | 15.8 |
| Agriculture/Livestock | 214 | 33.5 | 203 | 31.8 |
| Own Business | 112 | 17.5 | 99 | 15.5 |
| Others | 44 | 6.9 | 43 | 6.7 |
| Support from Family/Relatives/Friends | 5 | 0.8 | 26 | 4.1 |
| Social Safety-net | 0 | 0.0 | 47 | 7.4 |
| No Income | 2 | 0.3 | 25 | 3.9 |
| Monthly Income | ||||
| <10,000 | 184 | 28.8 | 428 | 67.0 |
| 10,001-20,000 | 266 | 41.6 | 166 | 26.0 |
| 20,001-30,000 | 113 | 17.7 | 32 | 5.0 |
| 30,001-40,000 | 40 | 6.3 | 06 | 0.9 |
| 40,001-50,000 | 26 | 4.1 | 05 | 0.8 |
| >50,000 | 10 | 1.6 | 02 | 0.3 |
| Average Income | 19,536.00 BDT | 10,638.00 BDT | ||
| Monthly Expenditure | ||||
| <5000 | 66 | 10.3 | 114 | 17.8 |
| 5,001-10,000 | 219 | 34.3 | 277 | 43.3 |
| 10,001-15,000 | 156 | 24.4 | 108 | 16.9 |
| 15,001-20,000 | 85 | 13.3 | 88 | 13.8 |
| 20,001-25,000 | 53 | 8.3 | 28 | 4.4 |
| 25,001-30,000 | 36 | 5.6 | 13 | 2.0 |
| >30,000 | 24 | 3.8 | 11 | 1.7 |
Discussion
According to this study, 432 respondents (67.6%) experienced health problems during the COVID-19 pandemic. Among them, physical illness (24.4%) and severe stress (33.1%) were the highest in number. One-third of the respondents (30.3%) did not access the health institution's services due to the fear of getting infected with COVID-19. Before the COVID-19 pandemic, 58.65% received service from private hospitals, which decreased by 16.35% during the pandemic. This is basically due to the unavailability of transportation (41.7%). Health systems around the world are overwhelmed with accumulative demand for COVID-19 care due to stigma, misperception, and restrictions on movement that disrupt health care services.5 The shortcomings of public health care have been exposed to a great extent, even in developing countries, such as Bangladesh.5 The pandemic has challenged the country's overall health care system, resulting in the mobilization of health-specific resources and diverting to combat the COVID-19-affected patients. The findings of our study showed that the accessibility rate of community clinics was 72.13% before COVID-19, and during COVID-19, it decreased by 36.84%. Similarly rural people's accessibility to government hospitals was 85.30% and 46.90% before and during the COVID-19 pandemic, practically identical to the situation for the private hospitals or clinics. Similar findings were found in Haiti, Lesotho, Liberia, Malawi, Mexico, and Sierra Leone, where both the supply and demand sides were disrupted and dropped to the use of MCH services.13,14
Regarding maternal and child health services, the same situation was found, with the majority 67.3% claiming that they did not access services due to fear of getting infected (37.4%) and unavailability of transportation (30.8%). In addition, a significant finding revealed that physicians were not present at their stations (13.5%) and 6% reported that health institutions were closed. It has a negative impact on getting treatment for pregnant mothers and child care when doctors were not available in the hospital or other institutions during COVID-19.14,15
Other than COVID-19 services, general health care services were disrupted, notably during the first stage of the lockdown. In most regions, the outdoor service was nearly closed. To prevent the virus from spreading, hospitals advised patients not to enter the hospital unless necessary.7
According to UNICEF, 116 million babies were estimated to be born during the COVID-19 pandemic, of which 2.4 million were born in Bangladesh.14 These babies are projected to be born up to 40 weeks after COVID-19, which currently straining health systems and medical supply chains all over the world, was recognized as a pandemic.14,15 The country ranks ninth in terms of the highest expected number of births for the period of 9 months during COVID-19.13 Countries with the highest expected numbers of births were India (20.1 million), China (13.5 million), Nigeria (6.4 million), Pakistan (5 million), and Indonesia (4 million).12,13 Most of these countries had high neonatal mortality rates even before the pandemic, and these levels may increase with COVID-19 conditions.14,15
Telemedicine is a new idea and technology that is emerging at a whirlwind speed. Physicians are also using this platform for their private practice as it has been recognized and legalized in many countries.22 During this COVID-19 crisis, when the buzzword is physical distancing, telemedicine takes on greater relevance, and in some cases it was the only option for a diseased person to communicate and consult with their physicians. People are using this because it reduces waiting time in hospitals and is easily accessible and cost- effective.22
The outbreak of the COVID-19 pandemic posed substantial barriers to diagnosis, treatment, and follow-up of chronic and critical diseases.17,23 Delivering regular and routine comprehensive care for chronic patients and emergency care was disrupted due to closures of health care facilities, shortage of public transportation, and reductions in services.24 COVID-19 is causing a major challenge for health care systems worldwide. Patients with weakened immune systems, such as chronic disease patients, are more prone to higher morbidity and mortality, and they contribute to a considerable proportion of the overall population, and appropriate management of these comorbidities is critical in mitigating the COVID-19.25
Different factors, such as the non-availability of drugs, poor diet adherence, and a lack of social support must be considered when managing chronic health conditions in future pandemics, because if immediate action is not taken, the economic impact of the disease could rise. 25 As a result of the health care system in developing countries, the management of the COVID-19 pandemic in these countries requires specific attention.
Strengths and Limitations of the Study
The working network of TMSS was the indirect strength of the study. However, social distancing, stigma, lockdown, and fear of COVID-19 infection were the challenges that the researchers faced in collecting data. Due to funding and labor constraints for COVID-19, data were collected from the Bogura Districts, its adjacent districts, towns, and villages, which comprise the largest of the center part of the northern region of Bangladesh.
Conclusion and Implications for Translation
The COVID-19 pandemic caused a significant disruption in the delivery of essential health services at a time when people needed them the most. Increased levels of illnesses, mental stress, financial instability, family suffering, physical damage, loss of family members, unintended abortions, and other apparent by-products of this disruption were identified by this study. However, there may be some long-term consequences, such as post-COVID-19 syndrome, that should be properly investigated, and some immediate and long-term remedies should be taken based on the evaluation to prevent any unforeseen future harm to those who survive the COVID-19 pandemic. This study also identified the situations and challenges in existing health care conditions and issues that will be evaluated to maintain health care services. Collaboration between the public and private sectors, as well as worldwide alliance are to combat COVID-19 and future pandemics. More large-scale and mixed- method studies are required to have an in-depth understanding of the impact of COVID-19, which will ultimately help the government, International and National Non-Government Organizations (NGOs), and policymakers in developing guidelines and strategies for dealing with future pandemics.
Compliance with Ethical Standards
Conflicts of interest:
The authors deciare no competing interests.
Financial Disclosure:
Nothing to deciare.
Ethics Approval:
This study was approved by the institutionai Ethicai Review Committee of the TMSS Medicai Coiiege, Bogura, Bangiadesh.
Disclaimer:
None.
Acknowledgments:
The authors would like to thank ail the staff of TMSS for their financial and technicai support in conducting this study. The authors wouid iike to acknowiedge Prof. Dr. Hosne Ara Begum, Professor Dr. Aiamgir Moudud Pavei, and coiieagues at the Heaith Sector, TMSS, for their support. The authors are gratefui to all the participants who provided vaiuabie data for this study.
Funding/Support:
There was no funding for this study.
References
- COVID-19 Weekly Epidemiological Update Edition 112 2022 Published October 5 (accessed )
- Early transmission dynamics in Wuhan, China of novel coronavirus- infected pneumonia. N Engl J Med. 2020;382:1199-1207.
- [CrossRef] [Google Scholar]
- Global COVID-19 case fatality rates. The Centre for Evidence-Based Medicine. Published March 17, 2020 (accessed )
- [Google Scholar]
- COVID-19 and Bangladesh: challenges and how to address them. Frontiers Public Health. 2020;8:154.
- [CrossRef] [PubMed] [Google Scholar]
- Media Statement: Knowing the Risks for COVID-19. WHO; Published March 08, 2020 (accessed )
- Countries test tactics in ‘war’ against COVID-19. Science. 2020;367(6484):1287-1288.
- [CrossRef] [PubMed] [Google Scholar]
- Bangladesh in virtual lockdown as coronavirus fight flares. Bdnews24.com. (accessed )
- [Google Scholar]
- Psychosocial and socio-economic crisis in Bangladesh due to COVID-19 pandemic: a perception-based assessment. Front Public Health. 2020;8:341.
- [CrossRef] [PubMed] [Google Scholar]
- Strategic assessment of COVID-19 pandemic in Bangladesh: comparative lockdown scenario analysis, public perception, and management for sustainability. Environ Dev Sustain. 2021;23(4):6148-6191.
- [CrossRef] [PubMed] [Google Scholar]
- The World Health Report 1006: Working Together for Health Published 2006 (accessed )
- The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health. 2011;9:3.
- [CrossRef] [PubMed] [Google Scholar]
- The Daily Star. Published April 29, 2020 (accessed )
- The effect of COVID-19 on maternal newborn and child health (MNCH) services in Bangladesh, Nigeria and South Africa: call for a contextualised pandemic response in LMICs. int J Equity Health. 2021;20(1):77.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnant Mothers and Babies Born During COVID-19 Pandemic Threatened by Strained Health Systems and Disruptions in Services. UNICEF. Published May 7, 2020 (accessed )
- [Google Scholar]
- The changing aspects of motherhood in face of the COVID-19 pandemic in low- and middle-income countries. Matern Child Health J. 2021;25(1):15-21.
- [CrossRef] [PubMed] [Google Scholar]
- Fear, hatred and stigmatization grip Bangladesh amid Covid-19 outbreak. The Business Standard. Published March 26, 2020 (accessed )
- [Google Scholar]
- Impact of COVID-I9 pandemic on chronic diseases care follow-up and current perspectives in low resource settings: a narrative review. int J Physiol Pathophysiol Pharmacol. 2021;13(3):86-93.
- [Google Scholar]
- Knowledge, attitude, practice, and fear of COVID-19: an online-based cross-cultural study. int J Ment Health Addict 2021:1-16.
- [CrossRef] [PubMed] [Google Scholar]
- Essential Services during COVID 19. MoHFW Government of India; Published 2020 (accessed )
- Student suicide risk and gender: a retrospective study from Bangladeshi press reports. int J Ment Health Add 2020
- [CrossRef] [Google Scholar]
- Psychological interventions for people affected by the COVID-19 pandemic. Lancet Psychiatry 2020:300-2.
- [CrossRef] [PubMed] [Google Scholar]
- Telemedicine and its scope in COVID-19: Commentary. Homœopathic Links. 2020;33(4):318-319.
- [CrossRef] [Google Scholar]
- Ineffective communicable diseases act helped spread of Covid-19. The Business Standard. Published April 22, 2020 (accessed )
- [Google Scholar]
- First COVID-19 suicide case in Bangladesh due to fear of COVID-l9 and xenophobia: Possible suicide prevention strategies. Asian J Psychiatr. 2020;51:102073.
- [CrossRef] [PubMed] [Google Scholar]
- Disruptions in maternal health service use during the COVID-l9 pandemic in 2020: experiences from 37 health facilities in low-income and middle-income countries. BMJ Glob Health. 2022;7(1):e007247.
- [CrossRef] [PubMed] [Google Scholar]





