Translate this page into:
Sex and Age-Based Differences in Adult Acute Myeloid Leukemia Hospitalizations in the United States, 2009-2018
✉Corresponding author email: deepa.dongarwar@bcm.edu
Abstract
Acute myeloid leukemia (AML) represents the fifth-worst five-year overall survival by cancer type in the United States, and the prognosis is shown to vary by age and sex. However, published data exploring temporal trends in the rates of hospitalization by sex and prognosis patterns incorporating both age and sex remains limited. Therefore, we investigated trends of acute myeloid leukemia (AML) hospitalization rates by sex and the differences in the AML hospitalization rates by sex and age in the adult population using the Nationwide Inpatient Sample database for the years 2009-2018. We examined the differences in rates of AML hospitalizations by sex and age. Next, we stratified the study duration into two groups of five years each: 2009-2013 and 2014-2018 and examined the differences in age and sex across the study period and groups. Pearson's chi-squared tests were conducted to determine the statistically significant differences in these bivariate comparisons. Overall, during the entire study period, we observed an increased rate of hospitalizations in males, when compared with their female counterparts. The highest AML hospitalization rate for both males and females was observed in the age group of 60-79 years; males accounted for 33.8 per 10,000 hospitalizations and females accounted for 23.3 per 10,000 hospitalizations. The greatest difference in hospitalization rates by age group and sex was observed in 18-39 years (males: 23.6 per 10,000 hospitalizations, females: 7.7 per 10,000 hospitalizations [p-value=<0.01]). The trend in the prevalence of AML hospitalizations by age or sex remains unchanged irrespective of the 5-year study period group. The results from this study would prove vital in directing the decision-making process for healthcare providers and AML patients alike as they work in tandem to navigate the complexities of AML and everything it entails
Keywords
Acute Myeloid Leukemia
Temporal Trends
Differences by Sex
Differences by Age
Join point Regression
HCUP NIS
Introduction
Acute myeloid leukemia (AML) is a heterogenous cancerous condition characterized by multiple cytogenetic abnormalities or chromosomal translocations that induce the likelihood of malignant transformation of hematopoietic progenitor cells.1,2,3 In the United States, the median overall survival of AML is 8.5 months representing the fifth-worst five-year overall survival by cancer type.3,4,5 AML primarily affects adults and has marked variability in prognosis that is based on multiple factors including molecular and genetic abnormalities, blast phenotype, age, sex, race, and socio-economic status.3,4,6 Extensive research has demonstrated, that of these factors, male sex consistently contributes to the least favorable prognosis.4,5 Males present an increased risk for developing AML after the age of 50 and this risk has been shown to continuously increase with age.4,5 However, published data exploring the differences in prognosis patterns incorporating both age and sex during the past decade (2009-2018) remains limited. In this study, we investigated the differences in the AML hospitalization rates by sex and age in the adult population during the study period.
Methods
Using Nationwide Inpatient Sample (NIS) data for the years 2009-2018 (the latest 10 years for which the data was available at the time of the study), we conducted this retrospective cohort study among all adult hospitalized patients in the United States (US). NIS is the largest all-payer inpatient care database in the US, containing information on about 35 million hospitalizations (weighted) each year.6 NIS uses complex survey design including strata, clustering, and weighting methodologies and presents a 20% sample of all hospitalizations in the US. NIS used the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-09-CM) to identify all the diagnoses and procedures related to each hospitalization till 2015, 3rd quarter, after which it transitioned to ICD-10-CM coding format. AML- associated hospitalizations were identified on the basis of the presence of any diagnosis code indicative of newly diagnosed, in remission, relapsed/refractory acute myeloid leukemia, and myeloid sarcoma (ICD- 9-CM: 205.0× for Myeloid leukemia acute, 205.3× for Myeloid sarcoma, 206.0× for Monocytic leukemia acute; ICD-10-CM: C92.0× for Acute myeloblastic leukemia, C92.3× for Myeloid sarcoma, C92.4× for Acute promyelocytic leukemia, C92.5× for Acute myelomonocytic leukemia, C92.A× for Acute myeloid leukemia with multilineage dysplasia, C93.0× for Acute monoblastic/monocytic leukemia).
We divided the study duration into two groups of 5 years each – 2009-2013 and 2014-2018. The rates of AML hospitalizations were calculated based on sex (female vs. male) and age groups: 18-39 years, 40-59 years, 60-79 years, 80+ years, overall and across the two study period groups. The differences in groups were examined using Pearson's chi-squared test. We used two-tailed hypothesis testing for all statistical analyses, and the type-1 error rate was set at 5%. We utilized R version 3∙5∙1 (University of Auckland, Auckland, New Zealand) and RStudio Version 1∙1∙5001 (Boston, MA) for performing all statistical analyses and the trends analyses were performed using Joinpoint Regression Program, version 4.7.0.0 (National Cancer Institute, USA). The study was implemented on de-identified publicly available data and therefore, was granted exempt status by the Institutional Review Board at Baylor College of Medicine, Texas, United States.
Results
There were a total of 305,617,638 hospitalizations during 2009-2018, out of which, AML hospitalization rates amounted to 2.2 per 10,000 hospitalizations. More specifically, 37,505 of these 67,915 AML hospitalizations (55.22%) were in males. It was determined that, overall, males exhibited about 1.7 times increased AML hospitalization rates than their female counterparts (males: 27.2 per 10,000 hospitalizations and females 16.0 per 10,000 hospitalizations). We observed a wide variability in AML hospitalization rates by age group. The highest hospitalization rate for both males and females was observed in the age group of 60-79 years. Within this age group, males accounted for 33.8 per 10,000 hospitalizations and females accounted for 23.3 per 10,000 hospitalizations. The hospitalization rate for males in the age group of 18-39 years was 23.6 per 10,000 hospitalizations, whereas, for females, it was 7.7 per 10,000 hospitalizations (p-value=<0.01), representing the greatest difference in hospitalization rates by age group and sex with a difference in the rate of 15.9 per 10,000 hospitalizations. The least difference in the AML hospitalization rates was found in the age group of 40- 59 years, (males: 23.7 per 10,000 and females: 22.8 per 10,000 hospitalizations). Overall, males consistently exhibited higher AML hospitalization rates than females for every adult age group that was examined (ages 18-39, 40-59, 60-79, and 80+) (Figure 1a). When stratified by 5-year study period, the differences in age groups were statistically significant (p-value=<0.01) with the highest hospitalization rates being in 60-79 (27.9 and 28.5 per 10,000 hospitalizations during 2008-2013 and 2014-2018 periods, respectively) years group (Figure 1b). Similarly, males had almost twice the AML hospitalization rates (about 27 per 10,000 hospitalizations) when compared with women (about 15 per 10,000) during both the 5-year study periods (Figure 1c).
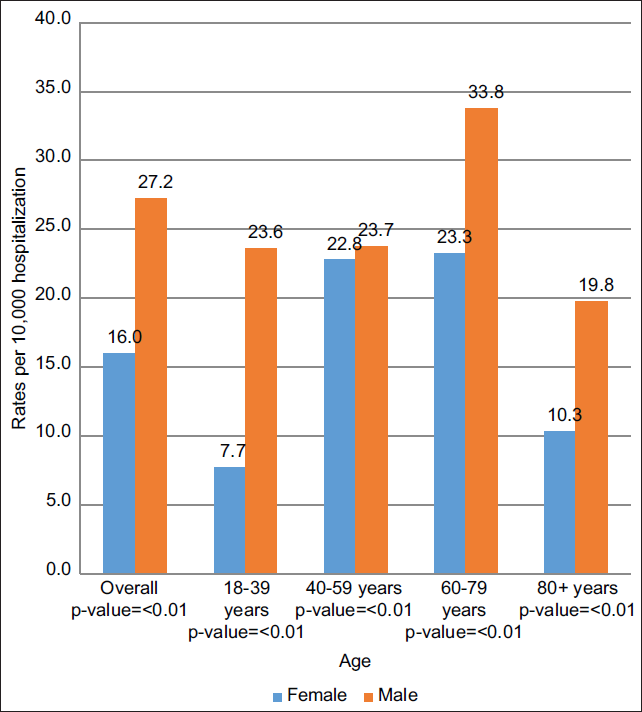
- Differences in acute myeloid leukemia (AML) hospitalization rates by sex and age during the entire study duration

- Differences in acute myeloid leukemia (AML) hospitalization rates by age and stratified by 5-year study period
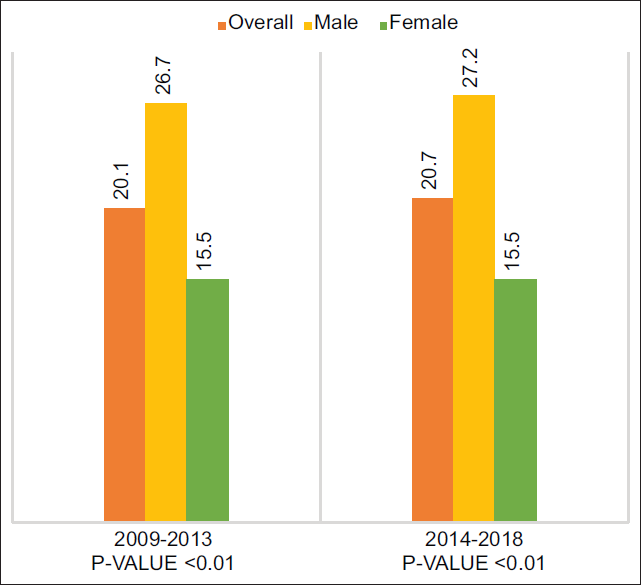
- Differences in acute myeloid leukemia (AML) hospitalization rates by sex and stratified by 5-year study period
Discussion, Conclusion, and Implications for Translation
Our results highlighted that among the multiple prognostic factors influencing AML, male sex consistently contributed to the least favorable prognosis. In general, compared to adult females, we observed higher AML hospitalization rates in the adult male population across ages 1880 years, with the most significant difference in the age group 60-79, where males exhibited the highest rate of AML hospitalizations in contrast to their female counterparts. We also observed that males belonging to the age group of 1839 years presented an AML hospitalization rate that was 3 times higher than females in the same age group. Our study findings confirm a previous study that showed an increased prevalence of AML hospitalizations in males than in females although the previous study was conducted in a pediatric population.7
It is important to take into account possible limitations to our findings. Firstly, the HCUP NIS has limited availability of clinical information that would have allowed for controlling the stage and grade of AML or patient characteristics such as the cytogenetic type of AML or age of diagnosis. Secondly, the disease severity can only be presumed by the number of hospitalizations, with a higher rate being possibly more indicative of a more advanced stage of AML; moreover, the NIS does not allow for examining readmissions in the same patients, since the information is unavailable in the dataset. However, these limitations are compensated by the very large sample size of the dataset and the extended duration of the study. This allowed us to explore and better characterize the sex differences affecting AML hospitalization rates. Future research should examine the genetic profiles of men with AML so as to determine what makes them more susceptible to less favorable AML outcomes. Conversely, future research could explore possible genetic factors that make women more amenable to less disease and better survival when it comes to AML. Regardless, the results from this study provide vital information needed in directing the decision-making process for healthcare providers and AML patients alike as they work in tandem to navigate the complexities of AML and everything it entails.
Compliance with Ethical Standards
Conflicts of interest:
None.
Financial Disclosure:
None.
Ethics Approval:
None as the study was performed on publicly available data.
Disclaimer:
None.
Acknowledgments:
None.
Funding/Support:
Research funding support was provided by the U.S. Department of Health and Human Services and Health Resources and Services Administration for Baylor College of Medicine Center of Excellence in Health Equity, Training, and Research (Grant No: D34HP3/024).
References
- Molecular biomarkers in acute myeloid leukemia. Blood Rev. 2017;31(1):63-76.
- [CrossRef] [PubMed] [Google Scholar]
- Sex disparity in childhood and young adult acute myeloid leukemia (AML) survival: evidence from US population data. Cancer Epidemiol. 2015;39(6):892.
- [CrossRef] [PubMed] [Google Scholar]
- Survival differences in childhood and young adult acute myeloid leukemia: a cross-national study using US and England data. Cancer Epidemiol. 2018;54:19.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of acute myeloid leukemia: recent progress and enduring challenges. Blood Rev. 2019;36:70-87.
- [CrossRef] [PubMed] [Google Scholar]
- Racial/ethnic, age and sex disparities in leukemia survival among adults in the United States during 1973-2014 period. PLoS One. 2019;14(8)
- [CrossRef] [PubMed] [Google Scholar]
- 2012. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality.
- In-hospital mortality and racial disparity in children and adolescents with acute myeloid leukemia: a population-based study. J Pediatr Hematol Oncol. 2022;44(1):e114-e122.
- [CrossRef] [PubMed] [Google Scholar]





