Translate this page into:
Prevalence and Associated Risk Factors of Postpartum Depression among Mothers in Pennsylvania, United States: An Analysis of the Pregnancy Risk Assessment Monitoring System (PRAMS) Data, 2012-2015
✉Corresponding author email: nluong@pa.gov
Abstract
Background:
Postpartum depression (PPD) is the most common morbidity among new mothers. With an estimated 140,000 resident births annually in the state of Pennsylvania, United States, no publication is available about the prevalence and risk factors associated with PPD specifically for Pennsylvania. This study aims to estimate the self-reported prevalence and risk factors associated with PPD.
Methods:
Weighted Pregnancy Risk Assessment Monitoring System (PRAMS) surveillance data of 4,022 Pennsylvania mothers with live birth(s) during 2012-2015 were analyzed. Descriptive statistics were used for mothers' characteristics. Between-group differences were evaluated using the Chi-square test. Risk factors associated with PPD were analyzed by logistic regression models. All analyses were performed using Stata version 13 (STATA Corp., College Station, TX), taking into account the complex survey design, and P-values <0.05 (2-tailed) were considered statistically significant.
Results:
Of the 4,022 mothers, the overall prevalence of PPD was 12.1% (515 mothers); the prevalence was 12.4% (108) in 2012,spiked to 14.8% (156) in 2013,then significantly declined to 10.9% (127) in 2014 and 10.1% (124) in 2015 (p=0.03). In a multivariable logistic model, significant risk factors included depression before pregnancy (adjusted odds ratio [aOR]: 3.7, 95% CI: 2.3-6.0), abuse before or during pregnancy (aOR: 3.5, 95% CI: 1.6-7.3), the mother's job loss (aOR: 2.1, 9S% Cl: 1.3-3.4), extended time away from husband/partner due to military deployment or work-related travel (aOR: 2.3, 95% CI: 1.1-4.5), a husband/partner not wanting the pregnancy (aOR: 1.7, 95% CI: 1.1-2.9), and arguing more than usual with a husband/partner (aOR: 1.6, 95% CI: 1.4-2.4).
Conclusion and Implication for Translation:
PPD is relatively common in Pennsylvania; however, the prevalence declined significantly during the study period. Depression before pregnancy, abuse before or during pregnancy, job loss, extended time away from husband/partner due to military deployment or work- related travel, husband/partner not wanting the pregnancy, or arguing more than usual with a husband/partner increased the odds of experiencing PPD. Further studies should be conducted on approaches to prevent PPD among new mothers.
Keywords
Depression
Postpartum Depression
Prevalence
Risk Factors
Surveillance
Pregnancy
Maternal Health
PRAMS
Introduction
Postpartum depression (PPD) is the most common morbidity among new mothers. PPD is associated with adverse infant and maternal health outcomes including lower breastfeeding initiation rates and early breastfeeding cessation,1,2 poor mother-child bonding and interactions,3,4 and infant developmental disorders or impaired child development.5,6 Murray et al. indicated children of mothers suffering from PPD are at higher risk of emotional, behavioral, and psychological problems as well as cognitive and language developmental delays in early infancy.7 Josefsson et al. indicated women with a history of PPD, if untreated, were approximately 6 times more likely to have recurrent depressive symptoms compared to those without PPD and they were also more likely to experience physical and mental illness later in life.8 Women with PPD should receive treatment as early as possible. Unfortunately, PPD is underrecognized and undertreated due to the stigma associated with this illness, mothers' lack of knowledge, and mothers' reluctance to use psychotropic medications during the breastfeeding period.9
Understanding the epidemiology of PPD is important for PPD detection, prevention, and control strategies. While there are unpublished data about the prevalence of PPD, no publication is available about PPD prevalence and risk factors contributing to PPD specifically for Pennsylvania. Results from this study are important for public health officials in Pennsylvania to estimate the burden of PPD for the large northeastern state with approximately 140,000 resident births annually, including sub-populations at a higher risk for PPD for targeted interventions. This study aims to determine the prevalence of PPD and identify potential risk factors associated with PPD among mothers who delivered live-born infant(s) in Pennsylvania.
Methods
Study Design and Population
Weighted data from the Pennsylvania Pregnancy Risk Assessment Monitoring System (PRAMS) phase 7 (years 2012-2015) were used for this analysis. PRAMS is an ongoing state-level, population-based surveillance system which gathers data on selected maternal behaviors, attitudes, and experiences before, during, and shortly after pregnancy. It is a joint research project conducted by participating states in collaboration with the Centers for Disease Control and Prevention (CDC)'s Division of Reproductive Health. PRAMS uses a complex survey design (multi-state stratified sampling) to capture information from higher-risk subpopulations. PRAMS is a mixed-mode mail and telephone survey. Since its implementation in 1987, PRAMS funding has expanded to 51 sites including Pennsylvania, and covers approximately 83% of all live births in the U.S.10,11 PRAMS data are weighted to adjust for noncoverage, nonresponse, different sampling rates in different strata, and to represent the total population of women with live birth(s) in Pennsylvania. Weighted response rates ranged from 65.3% to 69.0% during 2012-2015 for Pennsylvania PRAMS.
Pennsylvania women who had a live birth during the surveillance period of 2012-2015 were eligible for inclusion. Women were sampled between 2 and 6 months after giving birth. The state's birth certificate file served as the sampling frame for identifying new mothers. Self-reported PPD was determined based on mothers' responses (“always”, “often”, “sometimes”, “rarely”, and “never”) to two core depressive symptom questions: 1) “since your baby was born, how often have you felt down, depressed, or sad?”; and 2) “since your baby was born, how often have you had little interest or little pleasure in doing things?” These two questions were validated for the screening of general depression12 and were adapted by CDC as a surveillance tool for self-reported PPD on PRAMS.10 Mothers who responded “always” or “often” to either question were classified as experiencing PPD. The postpartum period was defined as the time between delivery and survey completion, which ranged from 2-9 months after delivery. Pennsylvania PRAMS was approved by the Pennsylvania Department of Health Institutional Review Board; Rutgers, The State University of New Jersey Institutional Review Board; and by the Centers for Disease Control and Prevention Institutional Review Board.
Statistical Methods
Weighted 2012-2015 Pennsylvania PRAMS surveillance data were analyzed. Descriptive statistics were used to describe the mothers' characteristics. Chi-square and/or Fisher's exact tests were used to determine between-group differences. The weighted prevalence of PPD was calculated based on the number of mothers who experienced PPD. PPD trend was evaluated using the Chi-square test for trend. Risk factors (demographic and clinical factors) associated with PPD were analyzed using logistic regression models with PPD as a dependent variable. Hosmer and Lemeshow stepwise strategies were applied for model building: potential independent variables with P-value <0.25 in the univariate logistic model were included in the initial full model.13 All analyses were performed using the Stata software (version 13; STATA Corp., College Station, TX), taking into account the complex survey design of PRAMS. P-values < 0.05 (2-tailed) were considered statistically significant.
Results
Prevalence of Postpartum Depression
A total of 4,022 women were identified as eligible during 2012-2015. The mean age was 29 years [inter-quartile range (IQR): 25-33], 79.2% of the population were in the age group of 20-34 years, and 72.0% were white. The overall prevalence of PPD was 12.1% (515 mothers); the prevalence was 12.4% (108) in 2012, spiked to 14.8% (156) in 2013, then significantly declined to 10.9% (127) and 10.1% (124) for 2014 and 2015 (p=0.03), Figure 1.
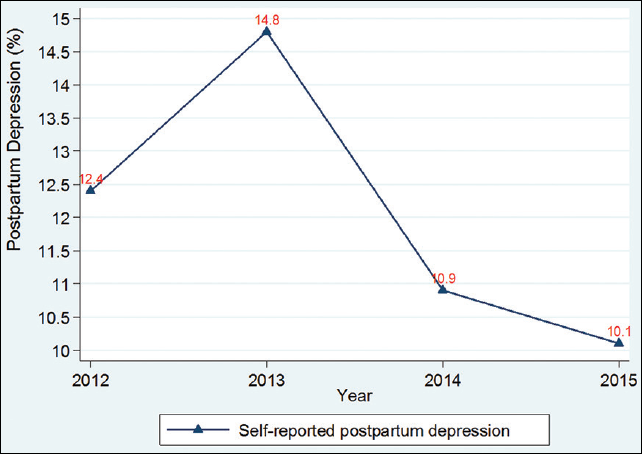
- Prevalence of postpartum depression (PPD), Pennsylvania, 2012-2015
Sociodemographic Characteristics
Demographic characteristics of the study population are presented in Table 1. Younger mothers experienced a higher prevalence of PPD: 19.8% of the mothers in the age group of ≤ 19 years experienced PPD, compared with 12.3% and 8.3% in the older age groups of 20-34 and ≥ 35, respectively (p<0.001). A significantly higher prevalence of PPD was reported in Black mothers (17.5%) compared with Asian (14.7%), White (10.9%), and mothers of other races (11.3%), respectively (p=0.004). Unmarried mothers or those with lower educational attainment or lower income reported a significantly higher proportion of PPD: 16.9% in unmarried versus (vs.) 8.6% in married mothers (p<0.001); 16.2% in mothers with a high school degree or below vs. 7.4% in mothers with a bachelor/higher degree (p<0.001); 21.1% in mothers with an annual income ≤$15,000 compared with 7.1% in mothers with income >$52,000 (p<0.001); and 17.0% in mothers who received WIC (the Special Supplemental Nutrition Program for Women, Infants, and Children) during pregnancy vs. 8.7% in mothers who did not receive WIC during pregnancy (p<0.001).
| Characteristic | No. of interviews (N, Column%) | PPD (N, Row %) | PPD (Column %) | P-value |
|---|---|---|---|---|
| Maternal age, year | ||||
| ≤ 19 | 203 (5.3) | 49 (19.8) | 8.7 | <0.001 |
| 20-34 | 3140 (79.2) | 400 (12.3) | 80.7 | |
| ≥ 35 | 677 (15.5) | 65 (8.3) | 10.6 | |
| Race | ||||
| White | 2929 (72.0) | 332 (10.9) | 65.1 | 0.004 |
| Black | 535 (13.6) | 103 (17.5) | 19.6 | |
| Asian | 143 (3.2) | 23 (14.7) | 4.0 | |
| Other* | 342 (9.5) | 46 (11.3) | 8.9 | |
| Unknown | 73 (1.7) | 11 (16.3) | 2.4 | |
| Ethnicity | ||||
| Non-Hispanic | 3606 (88.9) | 465 (12.3) | 90.4 | 0.56 |
| Hispanic | 374 (10.2) | 44 (10.7) | 9.0 | |
| Unknown | 42 (0.9) | 6 (8.9) | 0.6 | |
| Marital status | ||||
| Unmarried | 1584 (41.8) | 292 (16.9) | 58.5 | <0.001 |
| Married | 2433 (58.1) | 222 (8.6) | 41.2 | |
| Unknown | 5 (0.1) | 1 (25.9) | 0.3 | |
| Education | ||||
| High school and below | 1357 (37.1) | 250 (16.2) | 49.7 | <0.001 |
| Some college/associate degree | 1095 (26.8) | 141 (12.6) | 28.0 | |
| Bachelor's or higher | 1542 (35.3) | 119 (7.4) | 21.8 | |
| Unknown | 28 (0.8) | 5 (7.6) | 0.5 | |
| Household income | ||||
| ≤ $15,000 | 713 (18.2) | 166 (21.1) | 31.8 | <0.001 |
| $15,001 -29,000 | 693 (18.4) | 99 (13.5) | 20.6 | |
| $29,001 -52,000 | 590 (15.3) | 86 (12.7) | 16.1 | |
| > $52,000 | 1699 (39.4) | 123 (7.1) | 23.3 | |
| Unknown | 327 (8.7) | 41 (11.5) | 8.2 | |
| Received WIC** during the most recent pregnancy | ||||
| No | 2503 (59.8) | 226 (8.7) | 43.1 | <0.001 |
| Yes | 1485 (39.4) | 282 (17.0) | 55.4 | |
| Unknown | 34 (0.8) | 7 (22.3) | 1.5 | |
*: American Indian, Hawaiian, Alaskan native, mixed-race
**: the Special Supplemental Nutrition Program for Women, Infants, and Children
Clinical Characteristics of Mothers Reporting Postpartum Depression
Clinical characteristics of the mothers reporting PPD are given in Table 2. Prior to the pregnancy, 12.4% (514 mothers) reported depression, 5% (233) reported hypertension, and 2.6% (109) reported diabetes. Mothers with prior depression or hypertension reported a significantly higher prevalence of PPD: 29% in mothers with prior depression vs. 9.6% in mothers with no prior depression (p<0.001); 20.8% in mothers with prior hypertension vs. 11.6% in mothers with normal blood pressure (p=0.003). Mothers with a baby born <2,500 grams had a significantly higher prevalence of PPD (18.2%), compared with mothers who delivered a baby born ≥ 2,500 grams (11.6%, p<0.001); mothers with a baby born <37 gestational weeks had a significantly higher prevalence of PPD (18.8%) compared with mothers with a baby born 38-42 weeks, (11.4%, p<0.001). No differences in PPD were detected when compared between types of delivery such as vaginal, vaginal-assisted delivery (vacuum, forceps), and Cesarean section delivery.
| Characteristic | No. of interviews (N, %) | PPD (N, Row %) | PPD (Column %) | P-value |
|---|---|---|---|---|
| Before getting pregnant, the mother had: | ||||
| Diabetes | ||||
| No | 3836 (97.4) | 488 (11.9) | 96.4 | 0.19 |
| Yes | 109 (2.6) | 17 (17.1) | 3.6 | |
| Hypertension | ||||
| No | 3716 (95.0) | 455 (11.6) | 91.3 | 0.003 |
| Yes | 233 (5.0) | 51 (20.8) | 8.7 | |
| Depression | ||||
| No | 3440 (87.6) | 357 (9.6) | 70.1 | <0.001 |
| Yes | 514 (12.4) | 150 (29.0) | 29.9 | |
| Previous baby born >3 weeks before their due date | ||||
| No | 1901 (88.0) | 234 (11.5) | 82.5 | 0.007 |
| Yes | 354 (12.0) | 60 (17.8) | 17.5 | |
| Baby born <2,500 grams at birth | ||||
| No | 2801 (92.9) | 312 (11.6) | 89.3 | <0.001 |
| Yes | 1221 (7.1) | 203 (18.2) | 10.7 | |
| Baby born <37 gestational weeks | ||||
| No | 3083 (91.6) | 355 (11.4) | 86.9 | <0.001 |
| Yes | 911 (8.4) | 156 (18.8) | 13.1 | |
| Parity (prior live birth) | ||||
| No | 1726 (40.7) | 219 (12.0) | 40.4 | 0.35 |
| Yes | 2288 (59.3) | 294 (12.1) | 59.6 | |
| Type of delivery | ||||
| Vaginal | 2533 (67.0) | 315 (11.9) | 66.0 | 0.71 |
| Vaginal instrument assisted | 120 (3.3) | 13 (10.3) | 2.8 | |
| Caesarean section | 1366 (29.7) | 187 (12.7) | 31.2 | |
| Other stressors that occurred during the 12 months before the baby was born | ||||
| Close family member was sick | ||||
| No | 2953 (73.6) | 344 (11.0) | 67.0 | 0.003 |
| Yes | 1042 (26.4) | 165 (15.0) | 33.0 | |
| Got divorced/separated | ||||
| No | 3731 (93.0) | 445 (11.3) | 87.5 | <0.001 |
| Yes | 270 (7.0) | 65 (21.5) | 12.5 | |
| Moved to a new address | ||||
| No | 2727 (67.1) | 298 (10.1) | 56.0 | <0.001 |
| Yes | 1270 (32.9) | 213 (16.2) | 44.0 | |
| Was homeless | ||||
| No | 3913 (97.6) | 486 (11.7) | 94.7 | <0.001 |
| Yes | 86 (2.4) | 24 (27.0) | 5.3 | |
| Husband/partner lost his job | ||||
| No | 3567 (89.0) | 421 (11.4) | 84.2 | 0.001 |
| Yes | 424 (11.0) | 89 (17.3) | 15.8 | |
| I lost my job | ||||
| No | 3578 (88.9) | 407 (10.4) | 76.7 | <0.001 |
| Yes | 411 (11.1) | 104 (25.3) | 23.3 | |
| Husband/partner/I had a cut in pay | ||||
| No | 3326 (83.0) | 385 (10.7) | 73.6 | <0.001 |
| Yes | 666 (17.0) | 126 (18.7) | 26.4 | |
| Extended time away from my husband/partner | ||||
| No | 3822 (95.8) | 477 (11.7) | 94.0 | 0.13 |
| Yes | 172 (4.2) | 30 (17.2) | 6.0 | |
| Argued more than usual with my husband/partner | ||||
| No | 3089 (76.9) | 287 (8.4) | 54.0 | <0.001 |
| Yes | 899 (23.1) | 222 (23.9) | 46.0 | |
| Husband/partner did not want me to be pregnant | ||||
| No | 3656 (91.4) | 416 (10.5) | 80.5 | <0.001 |
| Yes | 333 (8.6) | 90 (27.2) | 19.5 | |
| Had problems paying bills | ||||
| No | 3229 (79.9) | 330 (9.3) | 61.8 | <0.001 |
| Yes | 768 (20.1) | 181 (22.9) | 38.2 | |
| Husband/partner/I went to jail | ||||
| No | 3829 (95.3) | 472 (11.5) | 91.3 | <0.001 |
| Yes | 159 (4.7) | 37 (22.2) | 8.7 | |
| Someone close had a problem with drinking/drugs | ||||
| No | 3493 (86.9) | 386 (10.3) | 74.3 | <0.001 |
| Yes | 504 (13.1) | 125 (23.7) | 25.7 | |
| Someone close died | ||||
| No | 3225 (80.4) | 386 (11.1) | 74.4 | 0.002 |
| Yes | 767 (19.6) | 124 (15.7) | 25.6 | |
All data are no. of patients (%) unless otherwise indicated
Risk Factors for Postpartum Depression
Several mothers reported other significant stressors occurring during the 12 months before the baby was born. Seven percent (270 mothers) reported a divorce/separation, 2.4% (86) reported homelessness, 11.1% (411) reported their job loss, 23.1% (899) argued more than usual with a husband/partner, 8.6% (333) reported a husband/partner not wanting the pregnancy, 20.1% (768) had problems paying bills, 4.7% (159) reported a husband/partner or the mother went to jail, 13.1% (504) reported someone close to them had a problem with drinking/drugs, and 19.6% (767) reported someone close to them died. Compared with mothers who did not encounter stressor(s), mothers with stressor(s) had a higher prevalence of PPD: 21.5% in divorced/separated mothers vs. 11.3% in non-divorced/separated mothers (p<0.001), 27% in homeless mothers vs. 11.7% in non-homeless mothers (p<0.001), 25.3% in those losing jobs vs. 10.4% in those who remained employed (p<0.001), 23.9% in mothers who argued more than usual with a husband/partner vs. 8.4% in mothers who did not argue more than usual (p<0.001), 27.2% in mothers who had a husband/partner not wanting the pregnancy vs. 10.5% in mothers who had a husband/partner wanting the pregnancy (p<0.001), 22.9% in mothers who had problems paying bills vs. 9.3% in mothers with no problem paying bills (p<0.001), 22.2% in mothers who or whose husband/partner went to jail vs. 11.5% in mothers who or husband/partner did not go to jail (p<0.001), 23.7% in mothers who reported someone close to them had a problem with drinking/drugs vs. 10.3% in mothers who said no one close to them had a problem with drinking/drugs (p<0.001).
Table 3 shows the selected demographic, clinical, and other predictors for PPD in the univariate and multivariate logistic regression analyses. Results from the multivariate model indicate the odds for developing PPD in mothers who had depression prior to the pregnancy were 3.7 times the odds in mothers who did not have depression [adjusted odds ratio (aOR): 3.7, 95% CI: 2.3-6.0]. Mothers who were abused before or during pregnancy had increased odds at 3.5 times higher than mothers who were not abused (aOR: 3.5, 95% CI: 1.6-7.3). During the 12 months before the baby was born: mothers who were apart from their husband/partner due to military deployment or extended work-related travel had increased odds at 2.3 times higher than the mothers who were not apart (aOR: 2.3, 95% CI: 1.1 -4.5); mothers who lost their jobs had increased odds at 2.1 times higher than those who did not (aOR: 2.1,95% CI: 1.3-3.4); mothers with a husband/partner not wanting the pregnancy had increased odds at 1.7 times higher than mothers whose husband/partner wanting the pregnancy (aOR: 1.7, 95% CI: 1.1-2.9); mothers who argued with their husband/partner more than usual had increased odds at 1.6 times higher than those who did not argue (aOR: 1.6, 95% CI: 1.4-2.4). Mothers ages ≥ 35 were less likely to report PPD (aOR: 0.6, 95% CI: 0.3-0.9) compared with mothers in the age group of 20-34 years. Significant predictors in the univariate model included being ≤19 years [odds ratio (OR): 1.8, 95% CI: 1.2-2.7], being Black (OR: 1.7, 95% CI: 1.3-2.3), being unmarried (OR: 2.2, 95% CI: 1.7-2.7), having lower educational attainment (had a high school degree or below, OR: 2.4, 95% CI: 1.8-3.1; had some college/associate degree, OR: 1.8, 95% CI: 1.3-2.4), having low income (income ≤$15,000, OR: 2.0, 95% CI: 1.4-2.8; income $15,001-29,000, OR: 1.9, 95% CI: 1.3-2.6; income $29,001-52,000, OR: 3.5, 95% CI:2.6-4.7), being abused before or during pregnancy (OR: 4.0, 95% CI: 2.6-6.0), having depression prior to pregnancy (OR: 3.8, 95% CI: 2.9-5.0), having hypertension prior to pregnancy (OR: 2.0, 95% CI: 1.3-3.0), having an unintended pregnancy (OR: 1.9, 95% CI: 1.4-2.3), having a baby born <37 weeks (OR: 1.8, 95% CI: 1.4-2.3), having a previous baby born <37 weeks (OR: 1.7, 95% CI: 1.1-2.4), having a baby born <2,500 grams (OR: 1.7, 95% CI: 1.4-2.0), and having stressor(s) during the 12 months before the baby was born (arguing more than usual with a husband/partner, OR: 3.4, 95% CI: 2.7-4.3; a husband/partner not wanting the pregnancy, OR: 3.2, 95% CI: 2.3-4.3; mother's job loss, OR: 2.9, 95% CI: 2.2-3.9).
| Predictors | Univariate | Multivariate |
|---|---|---|
| Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Maternal age, year, reference: 1=age group 20-34 years | ||
| ≤ 19 | 1.8 (1.2-2.7) | 1.6 (0.4-6.0) |
| ≥ 35 | 0.6 (0.4-0.9) | 0.6 (0.3-0.9) |
| Race, reference: 1=White | ||
| Asian | 1.4 (0.8-2.4) | 1.9 (0.8-4.8) |
| Black | 1.7 (1.3-2.3) | 1.3 (0.8-2.2) |
| Others* | 1.1 (0.7-1.5) | 0.5 (0.3-1.1) |
| Marital status, reference: 1=Married | ||
| Unmarried | 2.2 (1.7-2.7) | 1.1 (0.7-1.7) |
| Education, reference: 1=had “a bachelor's degree or higher” | ||
| High school and below | 2.4 (1.8-3.1) | 1.6 (0.9-2.8) |
| Some college/associate degree | 1.8 (1.3-2.4) | 1.3 (0.8-2.3) |
| Household income, reference: 1=income > $ 52,000/year | ||
| $29,001-52,000 | 3.5 (2.6-4.7) | 1.2 (0.7-2.1) |
| $15,001-29,000 | 1.9 (1.3-2.6) | 0.9 (0.5-1.6) |
| ≤ $15,000 | 2.0 (1.4-2.8) | 1.1 (0.6-2.0) |
| Depression before got pregnant, reference: 1=No | ||
| Yes | 3.8 (2.9-5.0) | 3.7 (2.3-6.0) |
| Abused before or during pregnancy, reference: 1=No | ||
| Yes | 4.0 (2.6-6.0) | 3.5 (1.6-7.3) |
| Diabetes before got pregnant, reference: 1=No | ||
| Yes | 1.5 (0.8-2.9) | 1.6 (0.5-5.2) |
| Previous baby born earlier than 3 weeks before their due date, reference: 1=No | ||
| Yes | 1.7 (1.1-2.4) | 1.3 (0.8-2.2) |
| Baby born<37 gestational weeks, reference: 1=No | ||
| Yes | 1.8 (1.4-2.3) | 1.2 (0.6-2.1) |
| Pregnancy intendedness, reference: 1=Yes | ||
| No | 1.9 (1.4-2.3) | 1.1 (0.7-1.6) |
| Baby born<2,500 grams at birth, reference: 1=No | ||
| Yes | 1.7 (1.4-2.0) | 1.1 (0.6-1.8) |
| Hypertension before got pregnant, reference: 1=No | ||
| Yes | 2.0 (1.3-3.0) | 0.6 (0.2-1.6) |
| Significant stressors that occurred during the 12 months before the baby was born, reference: 1=No | ||
| I was apart from my husband/partner due to military deployment or extended work-related travel | 1.6 (0.9-2.6) | 2.3 (1.1 -4.5) |
| I lost my job | 2.9 (2.2-3.9) | 2.1 (1.3-3.4) |
| Husband/partner did not want me to be pregnant | 3.2 (2.3-4.3) | 1.7 (1.1 -2.9) |
| I argued more than usual with my husband/partner | 3.4 (2.7-4.3) | 1.6 (1.4-2.4) |
*: American Indian, Hawaiian, Alaskan native, mixed-race
Discussion
The impact of PPD is deleterious to the mother, developing infant, and family when it is unrecognized and untreated.14,15 Our study aimed to determine the prevalence and identify potential risk factors associated with PPD among new mothers in Pennsylvania.
We reported the overall PPD prevalence of 12. 1 % for the entire period of 2012-2015: the prevalence was 12.4%, 14.8%, 10.9%, and 10. 1% for 2012, 2013, 2014, and 2015, respectively. This is higher than the 2012 overall national prevalence of 11.5% reported by Ko and colleagues.16 PPD can be severe and symptoms can be experienced up to 12 months after delivery.17 Findings from recent studies indicate declines in the prevalence of PPD in recent years.16,18 For example, Ko et al. reported a decline in the prevalence of PPD from 14.8% in 2004 to 12.6% in 2008, then to 9.8% in 2012 for 13 U.S. states; and the overall prevalence of PPD was 11.5% in 2012 for 27 U.S. states.16 Our results support this conclusion overall despite a small spike in 2013. Possible factors contributing to the recent decline in PPD include better identification of risk factors for depression and improved screening and treatment before and during pregnancy. Given an estimate of 140,000 live births per year and a PPD prevalence of 12.1%, the annual burden of PPD in Pennsylvania is around 16,940 mothers. Our unpublished data (PRAMS phase 7, years 2012-2015) indicate that 57.7% of pregnancies in Pennsylvania are unintended and unintended pregnancy increased the risk for PPD.19 The high number of new mothers suffering from PPD, in addition to the high rate of unintended pregnancy, suggest increased awareness of PPD is a key first step to tackle PPD.
Findings from recent studies show depression in the prenatal period was an independent predictor of PPD.20,21,22 Our findings further confirm women with depression before getting pregnant were approximately four times more likely to suffer from symptoms of PPD compared with those who did not have depression, suggesting screening for depression during prenatal care visits, postpartum visits, or during the infant's well-child visit is critical among new mothers, especially among those who have a history of depression. The American College of Obstetricians and Gynecologists (ACOG) suggests screening for PPD as an essential part of the mother's 4-6 week postpartum visit, and women can also be screened by pediatricians at their infants' well-child visits; health care providers screen for a mother's depressive symptoms at least once during pregnancy or postpartum, using a validated screening tool.23 In our study, 12.4% of the interviewed mothers reported depression before getting pregnant. This high prevalence in combination with a 4-fold increased risk for PPD among mothers with a history of depression suggests a critical need for timely screening, proper referral, and appropriate treatment for depression for Pennsylvania women during pregnancy and the postpartum period. The U.S. Preventive Services Task Force recommends all pregnant and postpartum women be screened for depression.24 In 2019, the American Academy of Pediatrics recommended screening of mothers for depression at the 1-, 2-, 4-, and 6-month well-child visits; that health care providers use community resources for the treatment and referral of the mother with depression; and provide support for the maternal-child relationship, including breastfeeding support.22
The association between PPD and being abused during or before pregnancy was reported in recent studies.18,20 Intimate partner violence can lead to severe complications including premature delivery, vaginal bleeding, miscarriage, physical injury, or death of the mother or infant.25 We defined “being abused before or during pregnancy” based on the responses to two questions regarding the time right before or during the most recent pregnancy: “During the 12 months before you got pregnant or during your most recent pregnancy, did your husband/partner push, hit, slap, choke, or physically hurt you in any other way?” Our data reported 3.8% of the women were abused, which is lower than a recent report of 6% by Chas et al.26 However, we found mothers who were abused during or before pregnancy had a 3.5-fold increased risk for PPD compared with mothers who were not abused, highlighting a need for routine screening of all women for intimate partner violence in Pennsylvania. Identifying women experiencing abuse and referring them to domestic violence services or programs is critical for PPD prevention.
Several stressors occurring during the 12 months before a new baby was born were examined in our study. These include (1) Partner- related stressors: e.g. argued with husband/partner more than usual, husband/partner did not want the pregnancy, separation or divorce from a husband/partner, extended time away from husband/partner; (2) Financial stressors: e.g. mother lost job, partner lost job, had problems paying bills; (3) Traumatic stressors: e.g. mother or husband/partner went to jail, was homeless; (4) Emotional stressors: e.g. family member was sick, someone close to the mother died. We found financial and partner-related stressors are significant and strong predictors for PPD. For example, mothers who reported “extended time away from husband/partner” had a 2.3 fold increased risk for PPD, “mother lost job” had a 2.1 fold increased risk, “partner did not want the pregnancy” had a 1.7 fold increased risk, and “argued with partner more than usual” had a 1.6 fold increased risk. These findings are consistent with reports from recent studies indicating life stressors within 12 months of giving birth were robust predictors for PPD27 and common life stressors during pregnancy were strongly associated with an increased prevalence of PPD, especially partner-related and financial stressors.28 The findings suggest women should be routinely screened during pregnancy for common stressors, then referred for support services in order to reduce or avoid PPD.
We observed the highest prevalence of PPD in women who are of younger ages (≤ 19 years old), unmarried, had a lower income (≤$15,000), had low educational attainment (high school degree or below), received WIC during pregnancy, had a baby born <2,500 grams, or who had a baby born < 37 weeks. The findings are consistent with results from the previous studies.16,18,21 Similarly to Salimi et al., we observed Black mothers had a higher proportion of PPD in comparison with other races,29 which is different from the finding reported by Ko et al. in the sample of 27 U.S. states where PPD was highest among mothers of American Indian/Alaska Native or Asian/Pacific Islander race/ethnicity.16
Women with PPD should receive appropriate treatment to avoid poor health outcomes. Josefsson et al. reported women with a history of untreated PPD were more likely to have recurrent depressive symptoms and experience physical and mental illness later in life, compared with those who did not have PPD,8 thus mothers who are considered to have self-reported PPD based on their screening should be administered a full diagnostic interview and receive early diagnosis and treatment. Women with the above risk factors should be targeted for PPD prevention and treatment.
Postpartum depression is a serious condition but treatable with pharmaco-and non-pharmacological therapy; however, it is often underdiagnosed and untreated. Ko et al. reported approximately 60% of women with depressive symptoms do not receive a clinical diagnosis and 50% of diagnosed women do not receive any treatment.30 Regardless of current treatments for PPD which are readily available, seeking help for PPD is underutilized.31,32,33 Stone et al. reported that only 38% of mothers with PPD sought help in their study.28 These data suggest that efforts toward early detection and referral of women with PPD to appropriate treatment are critical and urgent to reduce the burden of PPD. In addition, primary care physicians must remain alert to the high prevalence of depression in women of childbearing age and embrace routine screening for depression. In Pennsylvania, Title V funds support three programs that screen pregnant and new mothers for depression: home visiting programs, depression screening during a well-child visit, and screening in group prenatal care. Given an estimate of nearly 17,000 mothers with PPD in Pennsylvania, similar models should be expanded focusing on mothers who are at an increased risk for PPD.
Our study has several limitations. First, our data were from Pennsylvania PRAMS, which are based upon self-report, and PPD was not confirmed by a physician diagnosis. In addition, screening questions used in the survey, although validated, have a sensitivity of 58% and a specificity of 85% compared with clinical assessments of major depressive episodes.34 This may have resulted in underestimating the true prevalence of PPD in Pennsylvania. Second, new mothers were asked about symptoms experienced since delivery. The time duration, from the point when symptoms appeared to the point when the mother was interviewed, may range from 2-6 months, so mothers might not have recalled exactly when depression occurred. If the occurrence of depression fell outside of the postpartum period and depression was reported as within the period, PPD prevalence may have been overestimated. Conversely, if the occurrence of depression fell within the postpartum period and depression was not reported, PPD prevalence may have been underestimated. Third, screening questions did not evaluate the severity of PPD; hence, we are not able to determine burdens for drug therapy versus non-drug therapy since many women may only need nonpharmacologic interventions such as psychotherapy, exercise, yoga, acupuncture, and enhanced social support. Finally, Pennsylvania PRAMS has limited data on other mental health aspects such as mental health treatment including antidepressant use, seeking help during pregnancy, or treatment when a mother was identified as having PPD or encountered stressors. Further studies may need to look at how mothers with PPD seek help or treatment as well as the impact of treatment in reducing PPD, particularly with diverse populations.
Conclusion and Implication for Translation
Our findings indicate that PPD is relatively common; however, its prevalence is declining in Pennsylvania. PPD occurs more frequently in mothers with certain characteristics such as pregnancy at a younger age, being Black, being unmarried, or having low income or low education. Depression before getting pregnant, being abused before/during pregnancy, and having life stressors during the 12 months before the baby was born, especially partner-related or financial stressors, are important risk factors for PPD. Routine depression screening with a validated tool during pregnancy, the postpartum period, and child-well visits, focusing on mothers with the above-mentioned characteristics is essential. Increased awareness of PPD is important and key step to tackle PPD. Screening of all women for intimate partner violence and life stressors within 12 months of giving birth is critical for PPD detection and prevention. Home visiting programs, depression screening during a wellchild visit, and screening in group prenatal care should be expanded in Pennsylvania, focusing on mothers with a higher risk of PPD.
Compliance with Ethical Standards
Conflict of Interest:
All authors have no conflict of interest to declare
Financial Disclosure:
The authors have no financial relationships relevant to this article to disclose.
Ethical Approval:
Pennsylvania PRAMS was approved by the Pennsylvania Department of Health Institutional Review Board; Rutgers, The State University of New Jersey Institutional Review Board; and by the Centers for Disease Control and Prevention Institutional Review Board.
Disclaimers:
The results and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Pennsylvania Department of Health, Commonwealth of Pennsylvania, the Centers for Disease Control and Prevention, and the U.S. Department of Health and Human Services. The data were presented at the 2019 City Match Maternal and Child Health Leadership Conference in Providence, Rhode Island, USA.
Acknowledgment:
None.
Funding/Support:
Pennsylvania PRAMS has been funded by the Centers for Disease Control and Prevention and the U.S. Department of Health and Human Services Health Resources and Services Administration Title V Maternal and Child Health Services Block Grant funds.
References
- Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatr. 2007;96(4):590-594.
- [CrossRef] [PubMed] [Google Scholar]
- Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep). 2007;153(153):1-186.
- [Google Scholar]
- Effects of early maternal depression on patterns of infant-mother attachment: A meta-analytic investigation. J Child Psychol Psychiatry. 2000;41(6):737-746.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal depression and parenting behavior: A meta-analytic review. Clin Psychol Rev. 2000;20(5):561-592.
- [CrossRef] [PubMed] [Google Scholar]
- Postpartum depression and child development. Psychol Med. 1997;27(2):253-260.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Arch Womens Ment Health. 2003;6(4):263-274.
- [CrossRef] [PubMed] [Google Scholar]
- Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 2. impact on the mother-child relationship and child outcome. Br J Psychiatry. 2003;182:420-427.
- [CrossRef] [PubMed] [Google Scholar]
- A follow-up study of postpartum depressed women: Recurrent maternal depressive symptoms and child behavior after four years. Arch Womens Ment Health. 2007;10(4):141-145.
- [CrossRef] [PubMed] [Google Scholar]
- Preventing postpartum depression: Review and recommendations. Arch Womens Ment Health. 2015;18(1):41-60.
- [CrossRef] [PubMed] [Google Scholar]
- PRAMS. CDC; Updated 2019 (accessed )
- The pregnancy risk assessment monitoring system (PRAMS): Overview of design and methodology. Am J Public Health. 2018;108(10):1305-1313.
- [CrossRef] [PubMed] [Google Scholar]
- Casefinding instruments for depression. two questions are as good as many. J Gen Intern Med. 1997;12(7):439-445.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal depression and child psychopathology: A meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1-27.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child Psychiatry Hum Dev. 2012;43(5):683-714.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in postpartum depressive symptoms - 27 states, 2004, 2008, and 2012. MMWR Morb Mortal Wky Rep. 2017;66(6):153-158.
- [CrossRef] [PubMed] [Google Scholar]
- Peripartum depression: Early recognition improves outcomes. Cleve Clin J Med. 2017;84(5):388-396.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of self-reported postpartum depressive symptoms--17 states, 2004-2005. MMWR Morb Mortal Wkly Rep. 2008;57(14):361-366.
- [Google Scholar]
- Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79(3):194-198.
- [CrossRef] [PubMed] [Google Scholar]
- The association between pregnancy intendedness and experiencing symptoms of postpartum depression among new mothers in the United States, 2009 to 2011: A secondary analysis of PRAMS data. Medicine (Baltimore). 2017;96(6):e5851.
- [CrossRef] [PubMed] [Google Scholar]
- The risk factors for postpartum depression: A population-based study. Depress Anxiety. 2017;34(2):178-187.
- [CrossRef] [PubMed] [Google Scholar]
- Antenatal risk factors for postpartum depression: A synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289-295.
- [CrossRef] [PubMed] [Google Scholar]
- The American College of Obstetricians and Gynecologists Committee Opinion No. 630. Screening for perinatal depression. Obstet Gynecol. 2015;125(5):1268-1271.
- [CrossRef] [PubMed] [Google Scholar]
- Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the US preventive services task force. JAMA. 2016;315(4):388-406.
- [CrossRef] [PubMed] [Google Scholar]
- Intimate partner violence victimization prior to and during pregnancy among women residing in 26 U.S. states: Associations with maternal and neonatal health. Am J Obstet Gynecol. 2006;195(1):140-148.
- [CrossRef] [PubMed] [Google Scholar]
- Intimate partner violence and utilization of prenatal care in the United States. J Interpers Violence. 2014;29(5):911-927.
- [CrossRef] [PubMed] [Google Scholar]
- Identifying women at-risk for postpartum depression in the immediate postpartum period. Acta Psychiatr Scand. 2004;110(5):338-346.
- [CrossRef] [PubMed] [Google Scholar]
- Stressful events during pregnancy and postpartum depressive symptoms. J Womens Health (Larchmt). 2015;24(5):384-393.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between postpartum depression and perinatal cigarette smoking: An analysis of PRAMS data. J Subst Abuse Treat. 2015;56:34-38.
- [CrossRef] [PubMed] [Google Scholar]
- Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005-2009.J. Womens Health (Larchmt). 2012;21(8):830-836.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for depression and help-seeking in postpartum women during well-baby pediatric visits: An integrated review. J Pediatr Health Care. 2012;26(2):109-117.
- [CrossRef] [PubMed] [Google Scholar]
- Early access and help seeking: Practice implications and new initiatives. Early Interv Psychiatry. 2011;5(Suppl 1):34-39.
- [CrossRef] [PubMed] [Google Scholar]
- Enablers and barriers to seeking help for a postpartum mood disorder. J Obstet Gynecol Neonatal Nurs. 2011;40(4):450-457.
- [CrossRef] [PubMed] [Google Scholar]
- Brief scales to detect postpartum depression and anxiety symptoms. J Womens Health (Larchmt). 2012;21(12):1237-1243.
- [CrossRef] [PubMed] [Google Scholar]





