Translate this page into:
The Role of Health Belief Model in HIV Screening Decision among International Students in the United States: A Pilot Study
Abstract
Objectives:
We sought to determine how the Health Belief Model (HBM) constructs relate to Human Immunodeficiency Virus (HIV) screening decisions among international students and which of the HBM constructs was most relevant in those screening decisions.
Methods:
We conducted a cross-sectional pilot study using an online survey of international students at Western Illinois University in the United States. Participants signed electronic informed consent. The online survey comprised of questions that assessed their sociodemographic characteristics, acceptance of HIV screening, and perceived knowledge of HIV. The survey also determined the role of perceived benefits, perceived threat, and cues to action in making HIV screening decisions among the study population.
Results:
Four hundred and ninety students were invited to participate in the survey out of which 185 responses were obtained. In all, 107(57.8%) were males, and 78(42.8%) were females. Most of the respondents were from Asia (64.9%) and Africa (24.9%). The prevalence of acceptance of HIV screening among international students was found to be 73.5%. About 90% of the participants perceived HIV screening to be beneficial to their health, and 76% of them would accept the screening because they were offered. The majority (83%) of participants who said that they would not accept HIV screening, were also not sexually active, and they did not think they could be susceptible to HIV
Conclusion and Implications for Translation:
Perceived benefits and cues to action were found to be the significant factors that informed the decision of people who accepted to be screened for HIV Perceived susceptibility informed the decision of those that rejected the screening. Caution is warranted in generalizing the findings from this study because of the limited sample size; however, we are confident that our findings are reproducible in a larger population context.
Keywords
HIV
HIV screening
Decision
Acceptance
Perceived Benefit
Perceived Threat
Perceived Susceptibility
Health Belief Model
International Students
Introduction
Background of the Study
Most new Human Immunodeficiency Virus (HIV) infections are acquired through sexual intercourse.1 HIV transmissions from persons unaware of their HIV status occur more commonly than those who are aware of their HIV status.2 People Living with HIV (PLHIV) who are aware of their HIV status are more likely to prevent transmission through behavioral changes than those unaware of their HIV status. In the United States, statistics show that out of the 1.2 million people living with HIV, 156,300 people do not know they are infected.1 It is estimated that about 45,000 people are diagnosed with HIV annually, and 30% of new infections are transmitted by people who are infected but are yet to be diagnosed.1
One of the behavioral theories with significant relevance to disease prevention is the health belief model (HBM). The HBM was first developed in the 1950s by social psychologists in the United States Public Health Service for preventive health behavior. The primary concern at that time was the failure of people to accept disease prevention or screening, which was to enhance early diagnosis of asymptomatic diseases. Although these preventive measures were provided at little or no cost to the people, the acceptance was still very low. This observation led to the development of a theory that could explain preventive health behavior. 3,4 The HBM was subsequently extended to include responses of individuals to disease symptoms and their behaviors towards diagnosis and treatment compliance.5,6
The HBM constructs also show that disease preventive action is based on individual perception.7 The perceptions include susceptibility to a disease condition (perceived susceptibility), the deleterious consequences of disease (perceived severity), positive outcomes that can be derived from a behavioral modification (perceived benefits), and the perceived negative factors that can affect their health actions (perceived barriers).7 Over the years, HBM scholars introduced two additional constructs. The first is called self-efficacy, which is the belief that the behavioral change is achievable despite the perceived barriers.8 Second, is the specific cues to action, which helps in behavioral modification.9 These cues to action can be internal or external. Symptoms of illnesses, exposure to screening, physician counsels, health education and social marketing efforts supporting behavioral modification are specific cues to action that have been recently considered.10
While HIV testing is paramount for those who are living with undiagnosed HIV to reduce the spread of the virus,1 their perception of susceptibility is equally vital for screening to be accepted. Undiagnosed HIV infections limit the effectiveness of HIV programs because testing is the entry point for HIV care and treatment.11,12 A high proportion of HIV infected young people remain undiagnosed despite the individual and public health benefits of HIV testing.13
Although the early diagnosis of HIV is important because it provides prompt access to treatment that prevents progression to AIDS, there is a disproportionate rise in the incidence of HIV among college students.14 This increasing incidence of HIV may be explained by the low perception of susceptibility among college students. The perception of HIV risk has been shown to increase with age among college students.15 There is limited evidence about the perception of HIV risk among international students, especially in the United States, where students from diverse nationalities pursue tertiary education. There is also no HIV screening policy for these international students. We anticipate that the provision of routine screening for international students may contribute to the overall HIV prevention in the United States.
Objectives of the Study
The objectives of this study were to: (1) determine how Health Belief Model constructs influence HIV screening decisions among international students, and (2) identify which of the HBM constructs is most relevant for HIV screening decisions.
Specific Aims and Hypothesis
Although there is a considerable variation in the burden of the HIV epidemic among countries and regions, the interactions among international students may increase the perception of susceptibility. Drawing upon the HBM, we hypothesized that the perception of international students about HIV may play a role in their acceptance of the screening. We aimed to conduct a pilot study of international students at Western Illinois University (WIU) regarding the role of HBM in HIV screening decisions. We anticipate that the findings from this study may inform a more robust study of international students that can lead to a policy-driven conclusion.
Method
We designed a pilot cross-sectional quantitative survey for international students at the WIU. The study was conducted during the spring semester of 2017 for three months' duration. The instrument was validated by conducting a pilot test among 10% of the expected sample size (18 students). All the respondents answered the survey, and they were added to the overall survey respondents during data collection. The responses of the 18 students confirmed the clarity of the survey content (content validity) and reliability of the instrument. The sample size was calculated using the Kish Leslie formula.16 We estimated a robust sample size of 174 participants, approximated to 180, using a power calculation based on an expected prevalence of 13% for HIV screening acceptance17 at a confidence interval of 95%.18
Survey questionnaires were distributed through an electronic medium using the email contacts of all the international students from the listserv of all international students available at the Center for International Studies. Survey Monkey19 was used to enhance easy access and response to the questions. There are 491 international students enrolled at WIU at the time of this study.20 They are comprised of males and females whose ages were mainly between 15 and 35 years old with the younger students in the undergraduate program, while the older students are in the graduate programs.
The study participants were selected out of the 491 international students enrolled at WIU by convenience sampling based on their responses to the survey instrument. Participants were eligible if they were international students enrolled at the institution and signed the written informed consent to participate in the study. Ethical approval was obtained from the University's Institutional Review Board (IRB). All respondents signed a written informed consent electronically.
Study Variables
The questionnaire consisted of three-sections with 25- item responses selected from a drop-down list menu. The first section consisted of the independent variables, which are the sociodemographic information of the respondents. The second section assessed the perceived knowledge of the students about HIV; the third section assessed the acceptance of HIV screening among the students; the fourth section identified the perceptions of the respondents about HIV screening as it affects their decisions. Essentially, these sections asked about the respondents' reactions to the HBM constructs: perceived susceptibility to HIV, the benefit of the screening, the barrier to the screening, perceived severity of the disease, and cues to action that can influence their decision to accept HIV screening. Figure 1 depicts the relationships between the HBM constructs.
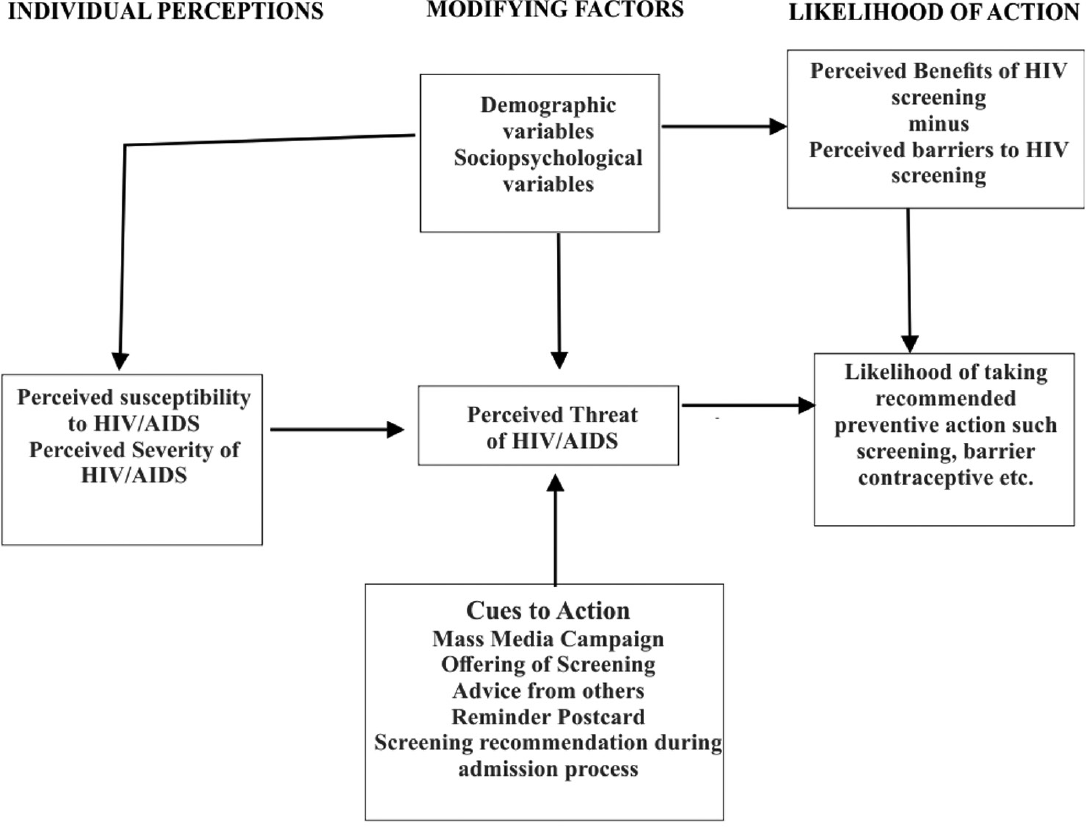
- The Health Belief Model Framework as a predictor of preventive health behavior (Adapted from Becker et al., 1974).
Statistical Analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) version 24.21 The baseline characteristics of the respondents were analyzed in a spreadsheet using a simple proportion of respondents. A chi-square test was done to explore associations between demographic characteristics, perceived knowledge, and acceptance of HIV testing. Logistic regression analysis was used to determine associations of the dependent variable (acceptance of HIV screening) with the independent variables. All levels of significance were set at p < 0.05.
Results
Sociodemographic Characteristics
A total of 185 respondents participated in the online survey, yielding a 38% response rate. Table 1 summarizes the sociodemographic characteristics of study participants. There were 107 (57.8%) males and 78 (42.8%) females (Table 1). A hundred and seventy-nine respondents (97%) were aged between 15 and 34 years, while 100 (54.1%) respondents were aged between 25 and 34 years. 149 (80.5%) and 28 (15.1%) respondents were full-time graduate and undergraduate students, respectively. Most of the respondents were single and never-married (73.0%), and 94 (50.8%) of them were not sexually active. Most of the respondents were from Asia (64.9%) and Africa (24.9%). One-third (33.5%) of the respondents were from India, while 17.3% were from Nigeria; in fact, most of the international students were from these two countries.
| Sociodemographic variables | Frequency N | Percentage (%) | |
|---|---|---|---|
| Gender | Female | 79 | 42.7 |
| Male | 107 | 57.8 | |
| Age | 15 to 24 | 79 | 42.7 |
| 25 to 34 | 100 | 54.1 | |
| 35 to 44 | 5 | 2.7 | |
| 45 to 54 | 1 | .5 | |
| 55 or older | |||
| Graduate International Student | Full time | 149 | 80.5 |
| Part-time | 5 | 2.7 | |
| Undergraduate International Student | Full time | 28 | 15.1 |
| Part time | 1 | .5 | |
| Employment status Family Income |
Employed, Graduate assistant | 54 | 29.2 |
| Employed, student worker | 59 | 31.9 | |
| Employed both Graduate assistant and student worker | 4 | 2.2 | |
| Not employed with the University but works within the United States with another organization | 6 | 3.2 | |
| Not employed at all | 60 | 32.4 | |
| Sexual activity | Yes | 88 | 47.6 |
| No | 94 | 50.8 | |
| Marital status | Married | 40 | 21.6 |
| Divorced | 1 | .5 | |
| In a domestic partnership or civil union | 3 | 1.6 | |
| Single, but cohabiting with a significant other | 5 | 2.7 | |
| Single, never married | 135 | 73.0 | |
| Continent of origin | Africa | 46 | 24.9 |
| Asia | 120 | 64.9 | |
| Australia | 1 | .5 | |
| Europe | 10 | 5.4 | |
| North America | 4 | 2.2 | |
| South America | 2 | 1.1 | |
| Departments | Natural Sciences | 33 | 17.8 |
| Social sciences | 10 | 5.4 | |
| Business | 24 | 13.0 | |
| Education | 15 | 8.1 | |
| Health Sciences | 21 | 11.4 | |
| Art | 3 | 1.6 | |
| Others | 77 | 41.6 | |
HIV Screening Decision
One hundred and thirty-six respondents accepted to do HIV screening if offered. Only 41 respondents refused HIV screening if offered, while 8 participants did not respond. Thus, the prevalence of acceptance of HIV screening among the study population is 73.5% (Table 2).
| HIV screening decisions | Reasons for respondents' decisions | Associated HBM* constructs | Frequency/percentage of respondents | Level of significance (p-value) |
|---|---|---|---|---|
| Accepted HIV screening (n = 136, 73.5% of 185) | Because of the screening benefit (n=123) | Perceived Benefit | 123 (90%) | 0.0000 |
| Because the screening was offered (n=l03) | Cues to Action | 103 (76%) | 0.0000 | |
| Refused HIV screening (n = 41, 22% of 185) | Because the screening benefit is unknown (n=41) | Perceived Benefit | 9 (22%) | 0.0000 |
| Because of the fear of screening procedure (needle pricks) | Perceived Threat | 11 (27%) | 0.0000 | |
| Because of not sexually active | Perceived Susceptibility | 34 (73%) | 0.0000 | |
| Because of the fear of stigmatization | Perceived outcome Severity | 8 (19%) | 0.0000 | |
*HBM- Health Belief Model
Figure 2 shows a bar graph presenting the association between the independent variable (country of origin) and the dependent variable (acceptance of HIV screening). Acceptance of HIV screening was highest among international students from the continents of Asia and Africa. However, there is no sufficient statistical power to determine any significant association between the continent of origin and HIV screening decisions because of the skewness of the study population (Figure 2).

- Acceptance of HIV screening and continent of origin of the respondents
Health Belief Model Constructs and HIV Screening Decisions
Table 2 and Figure 3 summarize the association between the HBM constructs and the HIV screening decisions. The two main significant HBM constructs associated with acceptance of the screening if offered, were the perceived benefit of the screening and the cues to action. Meanwhile, the refusal of HIV screening was associated with perceived susceptibility, perceived outcome severity, perceived threat and perceived benefit of the test (Figure 3).
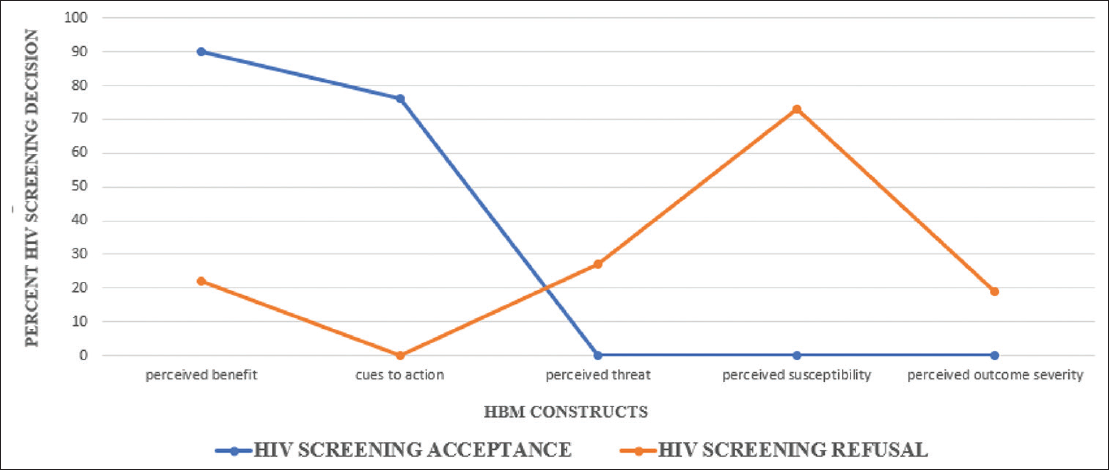
- HBM Constructs and HIV screening decisions
Perceived Benefit
Ninety percent (90%) of the respondents reported that they would accept HIV screening if offered. They said they made this decision because of their perceived benefit of HIV screening. They found HIV screening to be beneficial to their health.
Perceived threat
The majority (83%) of the respondents who reported that they would not accept HIV screening were also not sexually active. They did not think they could be susceptible to HIV infection.
Cues to action
In all, 76% of the respondents accepted the screening because it was offered. Offering HIV screening to these respondents was a cue to action for HIV screening.
Discussion
Application of Health Belief Model to the Acceptance of HIV Screening
Our study found a relevant application of the constructs of HBM to address behavioral attitude towards disease prevention.3,4 The HBM suggests that the responses of individuals to health promotion or disease prevention strategies are based on the following: the individual's belief that they are at risk of developing a specific condition; the belief that the risk is severe and has undesirable consequences; the belief that a specific behavior change will offer a benefit that leads to reduction of the risk; and the belief that one can overcome the barriers to the behavior change.22
The perceived threat is the first condition in the HBM. There are two types of perceived threats: perceived susceptibility and perceived severity. Susceptibility refers to how much risk a person perceives he or she has; severity refers to how serious the consequences might be. Perceived benefit is the belief that a behavioral change will be beneficial to the health of an individual. The self- efficacy is the belief that an individual is confident in his or her ability to make a behavioral change. The cues to action are considered necessary in assisting all stages of change in this model. A cue for action is what motivates behavior. In our study, for instance, the offering of HIV screening to the international students was the cue to action, while the acceptance of the screening was based on their self-efficacy. Becker et al. 23 described this model, and we adapted his description to create an algorithm for HIV screening (Figure 1).
Some studies have shown the applicability of the HBM in behavioral changes.24,25 Perceived benefit and perceived susceptibility were found to be the most important predictors of behavioral change. Our finding agrees with that of Kabiru et al. 24 In a study conducted on the correlates and motivations for HIV testing among youth in an urban settlement in Kenya, they reported that perceived risk for HIV infection may drive testing among youth. For example, about half of the youth who had ever had sex but had never been tested reported that they had not been tested because they were not at risk. Similarly, in a study conducted by Buldeo and colleagues exploring the HBM and first-year students' responses to HIV/ AIDS and voluntary counseling and testing (VCT) at a South African University, some students did not access VCT because of their low individual risk perception for HIV due to sexual abstinence.26 Based on our findings, we propose that with more cues to action, more people would be willing to screen for HIV, and those found to be positive would want to proceed to treatment. We, therefore, adapted the HBM to create an algorithm that can be used to describe the relevance of this theoretical framework in HIV screening (Figure 1).
Limitations and Feasibility
While we cannot generalize the findings from our study because of the small sample size, our study forms a pilot to inform the design of a multicenter study of international students in the United States. With the internal validity of our study, our findings are reproducible, and our survey instruments are replicable. There was a significant skewness of our population to the continents with the highest number of international students in the institution of this study. Perhaps, if the international students were evenly distributed from all the six continents assessed, we would be able to have a statistical significance relating to their countries of origin. Since this study is about international students, it is, however, challenging to have all continents evenly distributed, but a larger sample size may help in solving this problem. The number of international students in this institution is relatively small, and that also reflected on the difficulties faced in using a random sampling method, hence convenience sampling. However, given that this is a pilot study, we anticipate that our findings will inform the decision of researchers to conduct a more robust study where there will be a possibility of random sampling that will generate enough statistical power. Due to the sampling limitations, we were unable to generate a statistical power for our logistic regression analysis. Nonetheless, we deemed it fit to report our findings in order to stimulate further interest in this area of research.
Further studies should explore the benefits of HIV screening and consider making it the focus of health education during the process of introducing the screening to international students. Similarly, further research should determine if those who accept HIV screening would uptake the screening and whether it might be necessary for better understanding the interface between accepting the screening and getting the screening done. Finally, a large multi-center study may be necessary to help inform a potential policy of offering HIV screening for college students, especially during admission screening programs.
Conclusion and Implications for Translation
HIV screening continues to be an effective preventive strategy for HIV transmission. Among many of the studies conducted on the acceptance of HIV screening, studies among students mostly demonstrate a high level of acceptance because the level of awareness and knowledge about the disease tend to be high among students. There is an increase in the awareness of HIV and HIV screening among international students from continents with high HIV prevalence, but further studies may be needed to affirm if this translates to high knowledge of HIV and HIV screening. Perceived benefits and cues to action significantly informed the decision of people who accepted to be screened for HIV while perceived susceptibility informed the decision of those that declined to screen. We are cautious in generalizing the findings from this study because of the limited sample size, but we are confident that our findings are reproducible in a larger population context. From our findings, health educators, public health workers, and program planners for HIV screening can infer potential applications of HBM constructs in designing and achieving disease prevention. We anticipate that with more focus on the perceived benefit of screening and providing cues to action (screening availabilities, screening publicity, etc.), there would be a significant increase in the early detection rates for HIV and more people would subsequently be treated.
Compliance with Ethical Standards
Conflicts of Interest:
The authors declare no conflict of interest.
Financial Disclosure:
None of the authors received any form of financial benefit from this project.
Ethics Approval:
The study was approved by the Western Illinois University Institutional Review Board (IRB).
Disclaimer:
None.
Acknowledgments:
The first author, Dr. Ayosanmi, conducted this study during his Master of Science degree program at Western Illinois University. He acknowledges the support of the graduate students at Western Illinois University during the 20I7/20I8 session while collecting the data for this study. The support of the Center for International Students at Western Illinois University is immensely appreciated.
Funding/Support:
There was no funding from any agency to carry out this study.
References
- Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention. HIV Testing
- [Google Scholar]
- A meta-analysis of high-risk sexual behaviour in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446-453.
- [CrossRef] [PubMed] [Google Scholar]
- The health belief model and HIV risk behavior change. Preventing AIDS: Theories and Methods of Behavioral Interventions 1994:5-24.
- [CrossRef] [Google Scholar]
- Findings and theory in the study of fear communications. Adv Exp Soc Psychol. 1970;5:119-186.
- [CrossRef] [Google Scholar]
- Kirscht JP The health belief model and illness behavior. . 1974;2(4):387-408.
- [CrossRef] [Google Scholar]
- The Health Belief Model and Personal Health Behaviors. Health Education Monographs. 1974;2
- [CrossRef] [Google Scholar]
- The health belief model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 2015;30(6):566-576.
- [CrossRef] [PubMed] [Google Scholar]
- Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175-183.
- [CrossRef] [PubMed] [Google Scholar]
- Health Behavior and Health Education: Theory, Research and Practice 2008:45-65.
- Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Brit J Health Psychol. 2010;15(Pt 4):797-824.
- [CrossRef] [PubMed] [Google Scholar]
- The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793-800.
- [CrossRef] [PubMed] [Google Scholar]
- Optimizing the engagement of care cascade: a critical step to maximize the impact of HIV treatment as prevention. Curr Opin HIV AIDS. 2021;7(6):579-58.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness of HIV status, prevention knowledge and condom use among people living with HIV in Mozambique. PLoS One. 2014;9(9):e106760.
- [CrossRef] [PubMed] [Google Scholar]
- Patterns of condom use among students at historically Black colleges and universities: implications for HIV prevention efforts among college-age young adults. AIDS Care. 2013;25(2):186-193.
- [CrossRef] [PubMed] [Google Scholar]
- HIV sexual risk behaviors and perception of risk among college students: implications for planning interventions. BMC Public Health. 2009;9(1):281.
- [CrossRef] [PubMed] [Google Scholar]
- Survey Sampling 1965
- Acceptance rate of HIV testing among women seeking induced abortion in Benin City, Nigeria. Afr J Reprod Health. 2004;8(2):86-90.
- [CrossRef] [PubMed] [Google Scholar]
- Indicators and Methods for Cross-Sectional Surveys of Vitamin and Mineral Status of Populations. The Micronutrient Initiative (Ottawa) and the Centers for Disease Control and Prevention (Atlanta) 2007:125-128.
- [Google Scholar]
- The Health Belief Model and prediction of dietary compliance: a field experiment. J Health Soc Behav. 1977;18(4):348-366.
- [CrossRef] [PubMed] [Google Scholar]
- Willingness of Iranian young adults to eat organic foods: application of the Health Belief Model. Food Qual Pref. 2015;41:75-83.
- [CrossRef] [Google Scholar]
- HIV/AIDS among youth in urban informal (slum) settlements in Kenya: what are the correlates of and motivations for HIV testing? BMC Public Health. 2011;11(1):685.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring the Health Belief Model and first-year students' responses to HIV/AIDS and VCT at a South African university. Afr J AIDS Res. 2015;14(3):209-218.
- [CrossRef] [PubMed] [Google Scholar]





