Translate this page into:
COVID-19 Pandemic: Face Mask Mandates, Hospitalization, and Infection Rates in the United States
✉Corresponding author email: earmstrongmensah@gsu.edu
-
Received: ,
Accepted: ,
Abstract
Face masks have been identified as one of the preventive methods for the control of the 2019 coronavirus disease (COVID-19). Although the World Health Organization (WHO) and the United States Centers for Disease Control and Prevention (CDC) recommend the universal use of face masks, there are controversies in the implementation of a national face mask mandate in the US. This commentary discusses the relationship between facemask mandates and key COVID-19 indicators such as infection rates and hospitalization rates in the US. It also summarizes some of the political issues surrounding the implementation of the national face mask mandate. We conducted an ecological study on the relationship between face mask mandates and key COVID-19 indicators. We searched PubMed and Google Scholar and reviewed 150 English articles related to face mask challenges in the US published from 2005 to 2021. We identified seven challenges associated with face mask wearing - conflicting messaging, individualism, denial, health consequences, lack of a national masking standard, concerns of African American males, and environmental issues. We found that North Dakota, a state without a face mask mandate had the highest COVID-19 prevalence of 13.3%. The mean prevalence for the highest top 10 ranked states without and with a face mask mandate was 11.1% and 10.5%, respectively. We also found that Florida, Arizona and Georgia, states without a face mask mandates, had the highest cumulative hospitalizations of 83,381, 58,670, and 57,911 hospitalizations, respectively. Alabama, Indiana, and Minnesota, which have face mask mandates, had the lowest hospitalization rates of 47,090, 47,787, and 26,651, respectively.
Keywords
COVID-19
Face masks
Prevention
COVID-19 hospitalization
Infectivity rates
Infection rates
Challenges
Mask mandate
United States
Introduction
Following its emergence in Wuhan Province, China, in December 2019, the coronavirus disease of 2019 (COVID-19) spread to various parts of the world including the United States (US) and is now a global pandemic. 1 As of March 202', there were about 120 million COVID-19 cases and over 2 million deaths globally, with the US accounting for over 29.5 million of those cases and approximately 535,000 of the deaths.2 To slow down COVID-19 transmission, the US, like many other countries, established preventive measures including the temporary closure of communities and institutions, hand washing, social distancing, the wearing of face masks, and most recently, vaccinations. With the emergency approval of three COVID-19 vaccines (Pfizer-BioNTech, Moderna, and Johnson and Johnson brands) by the US Food and Drug Administration, mass vaccinations are underway in the US. While vaccines have thus far shown promise, the US Centers for Disease Control and Prevention (CDC), the nation's leading public health agency, recommends the continued wearing of face masks in public places as well as the continued observance of the other COVID-19 precautionary prevention measures as only 19% of Americans have been fully vaccinated3 and given the fact that it takes about 2-4 weeks for antibodies against the virus to be built. Irrespective of the recommendation, some Americans have refused to wear face masks. Reasons proffered include conflicting messaging, the lack of a national masking standard, individualism, denial, and health consequences associated with mask-wearing among others.4-6 These factors pose substantial challenges to COVID-19 prevention in the US.
We conducted an ecological study on the relationship between face mask mandates and key COVID-19 indicators such as hospitalization and infection rates in the US. We searched PubMed and Google Scholar and reviewed 150 English articles related to face mask challenges in the US published from 2005 to 2021. We conducted our search using a combination of keywords including COVID-19, face masks, prevention, challenges, mask mandate, and United States. Thirty-nine articles met our study's inclusion criteria. COVID-19 data on the prevalence, infectivity rate (the rate at which an infected person is able to spread the virus to another), current or cumulative number of hospitalizations, and deaths/100,000 population were obtained from the websites of all 50 State Health Department and the District of Columbia. These data were used to situate the challenges associated with face mask wearing in the US. This commentary discusses the relationship between facemask mandates and key COVID-19 indicators such as infection rates and hospitalization rates in the US. It also summarizes some of the political issues surrounding the implementation of the national face mask mandate.
Face Masks
Until recently, there were debates on whether face masks should be worn in public places in the US during the COVID-19 pandemic.7 Although initially of a different opinion, the CDC and the World Health Organization (WHO) recommend the wearing of face masks in public places as part of precautionary measures to control COVID-19 transmission.8 Presently, only children under the age of two and people with respiratory conditions are exempt from wearing face masks in the US.9
Face masks are personal protective equipment that can block the transmission of pathogens (bacteria and viruses) in the respiratory droplets and aerosols of an infected person from entering the nose and mouth of an uninfected person. They must conform to the face's contours and leave no gaps on the top, sides, or bottom of the face. Face masks must cover the face from the bridge of the nose to under the chin and should be loose but secure enough to stay in place. Once worn, shifting around, and pulling down to breathe or talk should be avoided, as doing this will reduce their efficacy.10
Types of Face Masks
There are many types of face masks. Those used in the US include full face masks (those worn over the whole face); half-face masks (those worn from below the eyes to below the chin); and quarter face masks (those worn from the top of the nose to the top of the chin). Regardless of the type, face masks may either be reusable or single use.
Reusable face masks
Cloth face masks are reusable masks made from an assortment of washable and reusable woven fabrics. Examples of cloth face masks are bandanas, t-shirt masks, neck gaiters (tube of fabric worn around the neck that can be adjusted to protect the face and neck), and balaclavas (tight-fitting garments that cover the head and neck).12 Cloth face masks made from cotton and blended with silk, chiffon, or flannel fabric, provide over 90% filtration efficacy.13 The best cloth face masks have multiple layers of woven breathable fabric. The double layers protect from the inhalation of the virus expelled by an infected person during respiration, coughing, sneezing, or even laughing. Reusable facemasks help to mitigate shortages caused by the surge in demand for disposable masks.
Disposable face masks
Disposable face masks are single-use masks that must be disposed of after use. Some examples of disposable face masks used in the US are the N95 respirator and the surgical mask, with the latter being the most commonly used by the general public. Irrespective of type, disposable face masks are usually made from polymers such as polypropylene, polyurethane, polyethylene, or polyester,14 and usually consist of three layers: (1) an inner layer, (2) a middle layer, and (3) an outer layer. While surgical masks can block the inhalation of large COVID-19 droplets and sprays, they cannot filter out all submicron-sized airborne particles or aerosols.15 This notwithstanding, evidence shows that surgical masks, just like cloth face masks, are helpful.15,16
Evidence that Face Masks Work
Few systematic reviews or meta-analyses have been conducted to examine the efficacy of face masks to protect against COVID-19 transmission. In a meta- analysis conducted in 2020, Li et al. reported that only six of the 5,158 articles they researched focused on the relationship between face face mask wearing, COVID-19 prevention, and diagnosis of COVID-19 by laboratories. Focusing on 1,233 participants from four countries; their study showed that wearing face masks significantly reduced the risk of COVID-19 infection (OR = 0.38, 95%CI = 0.21 – 0.69).17
Regardless of the paucity of studies on face mask efficacy and COVID-19 transmission, evidence from studies on other respiratory conditions transmitted like COVID-19, have found face masks to be effective. In a 2007-2008 cluster-randomized intervention study conducted during the influenza season to assess the effectiveness of face masks among 1,178 university students in the US, researchers found a significant reduction (up to 75% OR = 0.25, 95% CI = 0.07 – 0.87) in influenza-like illness (ILI).18 In this study, participants were put into three groups: (i) those wearing a face mask and practicing hand hygiene, (ii) those wearing only a face mask, and (iii) those engaging in no intervention. After six weeks of observations, the researchers found reduced ILI cases of influenza in the intervention groups that wore masks and practiced hand hygiene and those that only wore face masks. In an observational study conducted among school children in Japan, Uchida et al. found that wearing face masks reduced influenza infection by up to 15% (OR = 0.859, 95% CI = 0.778 – 0.949).19 In 2010, Larson et al. conducted a randomized trial of 509 Hispanic households on the incidence and secondary transmission of influenza. The households were divided into three groups: (i) educated with no access to alcohol-based hand sanitizer and face masks, (ii) educated with access to alcohol-based hand sanitizer, and (iii) educated with access to alcohol-based hand sanitizer and face masks. Participants in each of the groups provided nasal swab samples to the researchers and reported on any ILI symptoms they had bi-weekly. After 19 months of follow-up, the researchers found that despite poor compliance with mask-wearing, mask- wearing was associated with reduced secondary transmission of influenza.20
Face Mask Challenges in the US
Amid the COVID-19 pandemic, face mask-wearing has become a catalyst for partisan political conflict and nationwide feuds.21 The refusal by some Americans to wear face masks has enraged compliant citizens who perceive such acts as appalling and the willful disregard of the mask mandate. The reasons for the refusal are many. We discuss a few in this section.
Conflicting Messaging
Some in the US refuse to wear face masks in public places due to conflicting and oppositional messages by some politicians and public health officials. The messages create doubt and confusion as they are presented as fact, in some instances, and then shot down as fiction on other occasions. When a sitting president declares COVID-19 a hoax and a leading member of his COVID-19 task force contradicts him, there is a conflict in messaging.22 According to existing literature, some states with Republican governors contributed to the conflicting messaging, leading to substantial variations among states and creating barriers to the handling of educational messages on mask-wearing.23
If the wearing of face masks is to be taken seriously in the US, then politicians and public health officials need to speak with one voice. Politicians need to trust that public health officials know what they are doing. They also need to refrain from talking about issues that they do not have adequate knowledge about. Doing this will avoid confusion, point people in the right direction, and in the process, save lives.
Individualism
Many American adults do not want to be told to wear a face mask. To them, doing this not only violates their constitutional rights (First Amendment), but also infringes upon their civil liberties. For others, wearing face masks is uncomfortable.4 A study of a large segment of the American population on COVID-19 and mask- wearing found that 40% of participants indicated that they did not wear masks because it was their right to decide on whether or not to wear one, while 24% of participants said they chose not to wear face masks because they found them to be uncomfortable.4
The public needs to be educated on the fact that mask mandates do not infringe upon individual liberties but rather give people the power to protect themselves, their loved ones, and the community from COVID-19. They also need to be sensitized about the fact that state governments have “police powers” that give them the authority to curtail certain liberties during emergencies in order to preserve public health, safety, and the general welfare of citizens.24 According to the CDC, people who do not feel comfortable wearing masks, can practice at home with different types of masks for short periods so they can identify and get used to the one(s) that suit them the best.25 In addition, there is a need to sensitize people about how the discomfort associated with wearing masks pales compared to what they could experience if they become infected with COVID-19.
Denial
Some people in the US find it difficult to accept the reality, depth, and seriousness of COVID-19.26 They do not believe that the disease is real and sometimes question the credibility of epidemiologic data. Doing this provides them with some sort of defense mechanism to cope with the situation. Unfortunately, denial often leads to the avoidance of the issue at hand. It causes people not to hear the facts, and not to follow safety and precautionary measures such as the wearing of masks in this case. In South Dakota, patients dying from COVID-19 were reported to have still maintained that COVID-19 did not pose a threat to life.6 They reportedly mocked nurses who were attending to them and asked why they were wearing masks.
Talking to people who are in denial of COVID-19 even if it makes them uncomfortable, is necessary. This interaction may give them the security they need to move forward and take action to protect themselves from exposure or from becoming the source of infection.
Health Consequences
Some people have cited health concerns and conditions in the US as reasons for not wearing face masks. According to these people, face masks obstruct and make breathing difficult and, on some occasions, trigger respiratory diseases like chronic obstructive pulmonary disease (COPD).27 In a recent study, Mo et al. reported an elevation in systolic blood pressure, partial pressure of carbon dioxide, bicarbonate, and base excess among COPD patients who wore face masks compared to those who did not wear face masks.28 However, results from other studies show that, in such situations, the human body adjusts and keeps oxygen levels where they need to be.
There is also the perception that using face masks to prevent COVID-19 can predispose one to other infections. According to this school of thought, if used masks are not properly disposed of, they can facilitate the transmission of airborne microbes like fungus and bacteria. In their study on the relationship between bacterial and fungal contamination on used surgical masks worn by hospital workers, Luksamijarulkul et al. reported high levels of bacterial contamination on the external surface areas of masks.29
Lack of a National Masking Standard
President Biden's administration has mandated face mask-wearing in public places under section 7902(c) of title 5 of the Executive Order on Protecting the Federal Workforce and Requiring Mask-Wearing.8 The purpose of the mandate is to protect the federal workforce and to ensure the continued provision of activities and services to the public.5 However, there are debates on whether the president has the authority to issue such a mandate. Attempts to enforce the presidential mask mandate have become an increasingly politicized and contentious issue. Indeed, as of March 2021,17 Republican states, including Georgia, Louisiana, and Michigan, lifted their mask mandates disregarding the executive order. At present, there is no national mask-wearing standard.
This means that the virus can be easily transmitted by people who live in non-mask-mandated states to states where masks are mandated. If all states adhere to a common standard, the chances are that the rate of transmission and infectivity will reduce as the requirements will be the same across the board. States and counties have the power to mandate mask use; however, political leanings have made this a challenge.
A study conducted by the CDC in Kansas in August 2020 to assess trends in COVID-19 incidence in counties with and without a mask mandate showed that, the 24 counties with mask mandates saw a daily decrease in COVID-19 cases (mean decrease = 0.08 cases per 100,000 per day; 95% CI = −0.14 to −0.03). In the same study, the CDC found that 81 counties that lifted their mask mandates experienced daily increases in COVID-19 cases (mean increase = 0.11 cases per 100,000 per day; 95% CI = 0.01–0.21).30 Similarly, the results of a study conducted by researchers at the Vanderbilt University's Department of Health Policy in October 2020, showed that COVID-19 deaths were twice as high in counties in Tennessee without mask mandates compared to counties with mandates.23 Data in Tables 1 and 2, obtained from state health department COVID-19 dashboards, show the relationship between COVID-19 prevalence, rate of infectivity, hospitalizations, and deaths by states with and without face mask mandates as of March 2021. During that period, North Dakota (a state without face mask mandate) had the highest COVID-19 prevalence of 13.3% (Figure 1) compared to Rhode Island (a state with face mask mandate) with 12.6% (Figure 2). The mean prevalence for the top 10 states without and with a face mask mandate was 11.1% (Table 1) and 10.5%, respectively (Table 2). The mean number of deaths across all states without and with a face mask mandate was about 169.2 deaths/100,000 population (Table 1) and 147.7 deaths/100,000 population, respectively (Table 2). The highest number of deaths per 100,000 population was 306/100,000 in Alaska (Figure 3, state without face mask mandate) compared to Rhode Island which had a death rate of 245 deaths/100,000 population (Figure 4). With regards to the top three states with the highest cumulative hospitalizations, Florida, Arizona, and Georgia, which do not have face mask mandates had 83,381; 58,670; and 57,911 hospitalizations respectively (Figure 5). Ohio, Idaho, and Alabama, which have face mask mandates had the lowest rates of 52,129; 47,787; and 47,090 respectively (Figure 6). Infectivity rates ranged from a low of 0.73 in Arizona, a state without face mask mandate (Figure 7), to a high of 1.26 in Michigan, a state with face mask mandate (Figure 8).
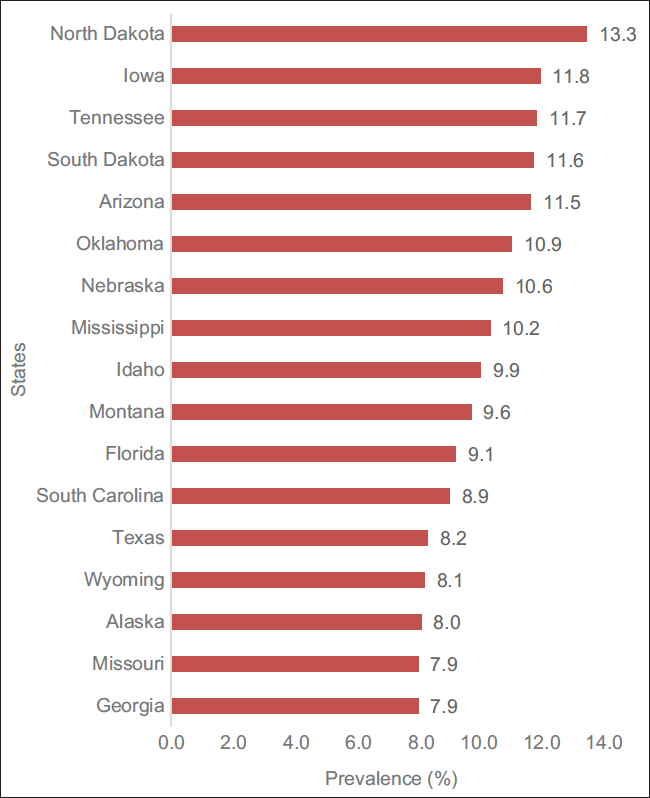
- Ranked COVID-19 prevalence in states without a face mask mandate

- Ranked COVID-19 prevalence in states with a face mask mandate

- Deaths per 100,000 population among states without face mask mandate

- Deaths per 100,000 population among states with face mask mandate.

- Cumulative number of hospitalizations in states with- out a face mask mandate
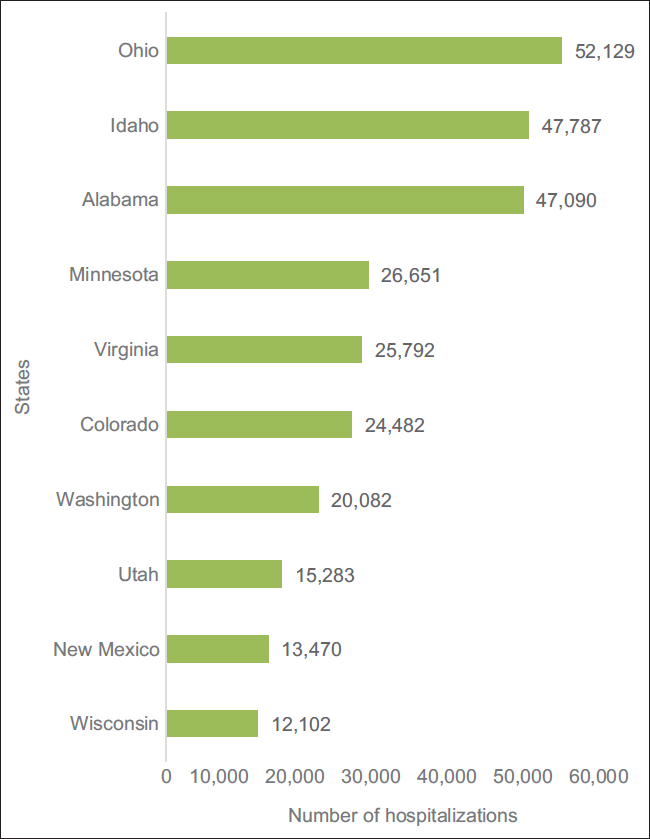
- Cumulative number of hospitalizations in states with a face mask mandate

- Infectivity rate of COVID-19 in states without face mask-wearing mandates

- Infectivity rate of COVID-19 in states with face mask-wearing mandates
| State | Population | Covid-19 Prevalence (%) | Infectivity Rate* | Hospitalizations** | Death/100,000 population | |
|---|---|---|---|---|---|---|
| 1 | Alaska | 731,545 | 8.0 | 1.00 | 37 (C) | 306 |
| 2 | Arizona | 7,278,717 | 11.5 | 0.73 | 58,670 (T) | 230 |
| 3 | Florida | 21,477,737 | 9.1 | 0.96 | 83,381 (T) | 152 |
| 4 | Georgia | 10,617,423 | 7.9 | 0.85 | 57,911 (T) | 152 |
| 5 | Idaho | l,787,065 | 9.9 | 1.05 | 7,434 (T) | 109 |
| 6 | Iowa | 3,155,070 | 11.8 | 0.96 | 174 (C) | 179 |
| 7 | Mississippi | 2,976,149 | 10.2 | 0.92 | 256 (C) | 234 |
| 8 | Missouri | 6,137,428 | 7.9 | 1.05 | 833(C) | 136 |
| 9 | Montana | l,068,778 | 9.6 | 1.05 | 4,716 (T) | 132 |
| 10 | Nebraska | l,934,408 | 10.6 | 0.97 | 133 (C) | 110 |
| 11 | North Dakota | 762,062 | 13.3 | 1.08 | 3,908 (T) | 192 |
| 12 | Oklahoma | 3,956,971 | 10.9 | 0.86 | 24,704 (T) | 121 |
| 13 | South Carolina | 5,148,714 | 8.9 | 0.92 | 542 (C) | 154 |
| 14 | South Dakota | 884,659 | 11.6 | 1.06 | 6,864 (T) | 217 |
| 15 | Tennessee | 6,833,174 | 11.7 | 0.99 | 19,338 (T) | 171 |
| 16 | Texas | 28,995,881 | 8.2 | 0.84 | 3,446 (C) | 161 |
| 17 | Wyoming | 578,759 | 8.1 | 0.93 | 22 (C) | 120 |
*Data obtained from covidactnow.org/?s=168315
Remaining data obtained from State Departments of Health
**C - current hospitalization, T - cumulative total hospitalization
Full list of data sources is available from the corresponding author upon reasonable request
| State | Population | Covid-19 Prevalence (%) | Infectivity Rate* | Hospitalizations** | Deaths/100,000 Population | |
|---|---|---|---|---|---|---|
| 17 | Alabama | 4,934,190 | 10.3 | 0.84 | 47,090 (T) | 212 |
| 18 | Arkansas | 3,017,825 | 10.9 | 0.85 | 216 (C) | 183 |
| 19 | California | 39,512,223 | 8.9 | 0.83 | 3,812 (C) | 142 |
| 20 | Colorado | 5,758,736 | 7.8 | 0.99 | 24,482 (T) | 107 |
| 21 | Connecticut | 3,565,287 | 8.3 | 1.05 | 204 (C) | 220 |
| 22 | Delaware | 973,764 | 9.4 | 1.02 | 110 (C) | 156 |
| 23 | District of Columbia | 705,749 | 6.1 | 0.94 | 139 (C) | 149 |
| 24 | Hawaii | 1,415,872 | 2.0 | 1.16 | 2,261 (T) | 32 |
| 25 | Illinois | 12,671,821 | 9.6 | 1.02 | 288 (C) | 166 |
| 26 | Indiana | 6,732,219 | 10.1 | 1.06 | 47,787 (T) | 186 |
| 27 | Kansas | 2,913,314 | 10.2 | 0.88 | 9,604 (T) | 166 |
| 28 | Kentucky | 4,467,673 | 9.4 | 0.92 | 490 (C) | 128 |
| 29 | Louisiana | 4,648,794 | 9.5 | 0.89 | 399 (C) | 215 |
| 30 | Maine | 1,344,212 | 3.6 | 1.08 | 1626 (T) | 54 |
| 31 | Maryland | 6,045,680 | 6.6 | 1.07 | 852 (C) | 132 |
| 32 | Massachusetts | 6,949,503 | 8.3 | 1.05 | 588 (T) | 237 |
| 33 | Michigan | 9,986,857 | 6.3 | 1.26 | 1294 (T) | 159 |
| 34 | Minnesota | 5,639,632 | 8.5 | 1.12 | 26,651 (T) | 120 |
| 35 | Nevada | 3,149,234 | 9.6 | 0.94 | 309 (C) | 164 |
| 36 | New Hampshire | 1,359,711 | 5.9 | 1.06 | 1,183 (T) | 90 |
| 37 | New Jersey | 8,882,190 | 8.6 | 1.07 | 1,961 (T) | 244 |
| 38 | New Mexico | 2,096,829 | 9.0 | 0.90 | 13,470 (T) | 185 |
| 39 | New York | 19,453,561 | 9.2 | 0.95 | 4.355 (C) | 205 |
| 40 | North Carolina | 10,488,084 | 8.5 | 0.95 | 964 (C) | 174 |
| 41 | Ohio | 11,689,100 | 8.6 | 0.97 | 52,129 | 157 |
| 42 | Oregon | 4,217,737 | 5.6 | 0.98 | 8,983 (T) | 56 |
| 43 | Pennsylvania | 12,801,989 | 6.7 | 1.06 | l,554 (T) | 194 |
| 44 | Rhode Island | 1,059,361 | 12.6 | 1.04 | 129 (C) | 245 |
| 45 | Utah | 3,205,958 | 11.9 | 0.95 | 15,283 (T) | 64 |
| 46 | Vermont | 623,989 | 2.8 | 1.00 | 22 (C) | 35 |
| 47 | Virginia | 8,535,519 | 7.1 | 0.99 | 25,792 (T) | 119 |
| 48 | Washington | 7,614,893 | 4.4 | 1.03 | 20,082 (T) | 68 |
| 49 | West Virginia | 1,792,147 | 7.7 | 1.09 | 198 (C) | 145 |
| 50 | Wisconsin | 5,822,434 | 9.8 | 0.98 | 12,102 (T) | 113 |
*Data obtained from covidactnow.org/?s=168315
Remaining data obtained from State Departments of Health
**C - current hospitalization, T - cumulative total hospitalization
Full list of data sources is available from the corresponding author upon reasonable 0request
A standard mask policy that requires universal mask-wearing is an essential component of a comprehensive strategy to reduce exposure to and transmission of COVID-19. Such efforts are significant, given the high rates of infectivity, hospitalizations, and deaths from the virus.31,32
Concerns of African American Males
A significant challenge to the wearing of face masks in the US is that some African American men are concerned that covering their faces may lead to their arrest or being shot by the police. They feel that wearing a mask is a more significant threat to their lives than COVID-19. Thus, they are hesitant to wear face masks.33 In a hardware shop in Chicago's South Loop, a 35-year-old African American male attorney who wore a face mask just as the other white shoppers, was stopped by the police when he was leaving the store with a cart.34 If the police continue to profile and target African American men in masks unfairly, chances are, they will further prevent this population from wearing face masks.
Environmental Issues
The increased demand for disposable face masks in the US has implications for pollution. The indiscriminate dumping of disposable surgical masks into water bodies threatens aquatic life35,36 as many marine species, confusing the masks for food, eat them, and end up dying.37
The US leads the world in daily medical waste generation, producing about 8,055 tons of medical waste per day during the pandemic.38 Studies documenting improper disposal of surgical masks found that a substantial amount of disposed surgical masks and gloves were retrieved from water bodies in Virginia—a state with face mask mandate—during the state's annual trash clean-up in 2020.39 The US Environmental Protection Agency advocates for proper dispossal of masks and gloves, it also cautions against dispossing them in the waterways.40
Conclusion and Implications for Translation
Wearing face masks contributes to the prevention of COVID-19 transmission. If the challenges in the US discussed are not addressed, chances are, it might take a while to reduce infectivity, transmission, hospitalization, and death rates. Consequently, we call for continued public health education on the importance of face masks and the implementation of a standard face mask mandate across all 50 states and Washington DC. Additionally, law enforcement agents should be educated on the need to stop profiling African Americans wearing face masks, so this population's legitimate fear of being queried or arrested for practicing COVID-19 prevention measures can be mitigated.
Compliance With Ethical Standards
Conflicts of Interest:
The authors declare no conflict of interest.
Financial Disclosure:
None declared.
Ethics Approval:
This study was based on existing literature.
Disclaimer:
None.
Acknowledgments:
None.
Funding/Support:
None declared.
References
- Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
- [Google Scholar]
- Coronavirus Disease 2019 (COVID-19): Situation Report, 88. Published April 2020 (accessed )
- States ranked by percentage of population. Becker's Hospital Review. Published 2021 (accessed )
- [Google Scholar]
- American individualism is an obstacle to wider masking wearing in the US. Brookings. Published August 2020 (accessed )
- [Google Scholar]
- Executive Order on Protecting the Federal Workforce and Requiring Mask-Wearing. The White House; Published January 2021 (accessed )
- ‘It's not real’. South Dakota, which has shunned masks and other COVID rules, some people die in denial, nurse says USA Today. Published November 2020 (accessed )
- [Google Scholar]
- Published February 2019 (accessed )
- Coronavirus Disease (COVID-19) Advice for the Public: When and How to Use Masks. Published December 2020 (accessed )
- This is why kid under 2 don't need face masks, according to the CDC Yahoo Life. Published May 2020 (accessed )
- [Google Scholar]
- Coronavirus face masks and protection FAQ. Johns Hopkins Medicine. Published January 2021 (accessed )
- [Google Scholar]
- Face masks: benefits and risks during the COVID-19 crisis. Eur J Med Res. 2020;25(1):1-8.
- [CrossRef] [PubMed] [Google Scholar]
- 9 types of masks and how effective they are. Healthgrades. Published November 2020 (accessed )
- [Google Scholar]
- Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14(5):6339-6347.
- [CrossRef] [PubMed] [Google Scholar]
- Technical textiles for protection. In: Scott RA, ed. Technical Textiles for Protection (1st). Cambridge, England: Woodhead Publishing; 2005.
- [CrossRef] [Google Scholar]
- Wearing surgical masks in public could help slow COVID-19 pandemic's advance. Science Daily. Published April 2020 (accessed )
- [Google Scholar]
- Reducing tuberculosis transmission: a consensus document from the World Health Organization Regional Office for Europe. Eur Respir J. 2019;53(6):1900391.
- [CrossRef] [PubMed] [Google Scholar]
- Face masks to prevent transmission of COVID-19: a systematic review and meta-analysis. Am J Infect Control. 2020;S0196-6553(20):31043-9.
- [CrossRef] [Google Scholar]
- Facemasks, hand hygiene, and influenza among young adults: a randomized intervention trial. PLoS One. 2012;7(1):e29744.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of vaccination and wearing masks on seasonal influenza in Matsumoto City, Japan, in the 2014/2015 season: An observational study among all elementary schoolchildren. Prev Med Rep. 2016;5:86-91.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of non-pharmaceutical interventions on URIs and influenza in crowded, urban households. Public Health Rep. 2010;125(2):178-191.
- [CrossRef] [PubMed] [Google Scholar]
- McKelvey T Coronavirus: Why are Americans so angry about masks? BBC News. Published July 2020 (accessed )
- [Google Scholar]
- The president vs. the doctor: Messages and tone conflict in a long-distance COVID-19 debate. USA Today. Published May 2020 (accessed )
- [Google Scholar]
- These states have COVID-19 mask mandates. U.S. News & World Report. Published April 2021 (accessed )
- [Google Scholar]
- State police powers: a less than optimal remedy for the COVID-19 disease. Rand Corporation; Published May 2020 (accessed )
- [Google Scholar]
- Guidance for Wearing Masks. Published April 2021 (accessed )
- Pandemic denial: Why some people can't accept Covid-19's realities. CNN Health. Published August 2020 (accessed )
- [Google Scholar]
- Face masks for the public during the covid-19 crisis. BMJ. 2020;369:m1435.
- [CrossRef] [PubMed] [Google Scholar]
- Risk and impact of using mask on COPD patients with acute exacerbation during the COVID-19 outbreak: a retrospective study. Res Square 2020
- [CrossRef] [Google Scholar]
- Microbial contamination on used surgical masks among hospital personnel and microbial air quality in their working wards:A hospital in Bangkok. Oman MedJ. 2014;29(5):346-350.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in county- level COVID-19 incidence in counties with and without a mask mandate—Kansas, June 1-August 23, 2020. Morb Mortal Wkly Rep. 2020;69(47):1777-1781.
- [CrossRef] [PubMed] [Google Scholar]
- Emergence of SARS-CoV-2 b.1.1.7 lineage—United States, December 29, 2020 - January 12, 2021. Morb Mortal Wkly Rep. 2021;70(3):95-99.
- [CrossRef] [PubMed] [Google Scholar]
- Variants of the Virus that Causes COVID-19. Published April 2021 (accessed )
- For black men, fear that masks will invite racial profiling. The New York Times. Published April 2020 (accessed )
- [Google Scholar]
- ‘Which death do they choose?’: Many Black mean fear wearing a mask more than the coronavirus. STAT. Published June 2020 (accessed )
- [Google Scholar]
- Covid-19 face masks: A potential source of microplastic fibers in the environment. Sci Total Environ. 2020;737:140279.
- [CrossRef] [PubMed] [Google Scholar]
- Environmental effects of COVID-19 pandemic and potential strategies of sustainability. Heliyon. 2020;6(9):e04965.
- [CrossRef] [PubMed] [Google Scholar]
- Single use vs. reusable face masks: What's the difference? Days Like Laura. Published October 2020 (accessed )
- [Google Scholar]
- Coronavirus disease 2019 (COVID-19) induced waste scenario: A short overview. J Environ Chem Eng. 2021;9(1):104660.
- [CrossRef] [PubMed] [Google Scholar]
- Improper disposal of PPE contributes to waste. Environmental Protection. Published January 2021 (accessed )
- [Google Scholar]
- EPA United States Environmental Protection Agency. Don't Let Your Masks and Gloves Become Pollution. Published April 2021 (accessed )
- [Google Scholar]





