Translate this page into:
Safety of Hyperbaric Oxygenation Treatment and Evaluation of Associated Clinical Parameters: A Single-Institutional Prospective Cohort Study
✉Corresponding author email: gonzalomongemartinez@gmail.com
Abstract
Background and Objective:
Adverse events (AEs) associated with hyperbaric oxygen therapy (HBOT) are uncommon and typically not serious, being the most frequent otic/sinus barotrauma. The objective of this study is to analyze the safety of the HBOT at 1.45 atmosphere absolute (ATA) and compare it with reports at the same and higher pressures of treatment.
Methods:
A total of 175 patients (68 male, 107 female) were included in this prospective study. All patients were treated with HBOT at our facility from December 2019 to August 2021. For the comparative analysis, reports from studies published from 2012 to 2021 in MEDLINE EMBASE, BIREME, Lilacs, Scielo, and the Cochrane library were used. Binary variables are described in percentages with a 95% confidence interval (95% CI). Inferential analysis was performed using a bivariate analysis by calculating odds ratio (OR) with 95% confidence intervals. Statistical analyses and sample size calculations were performed with Stata version 13.0 (College Station, TX, USA).
Results:
In this study, the AE per session was 7.1% for total AE and 4.1% for overall barotrauma. AE was reported in 28.3% of patients (n=49), with barotrauma and non-barotrauma AE in 20.3% (n=35) and 8.1% (n=14), respectively. All barotrauma was recorded as subjective (100% of ear ache without eardrum damage, Teed scale=0). The frequency of total AE obtained in our study was statistically higher for 1.5, 2, and >2 ATA. Non-barotrauma AE was also higher, but objective barotrauma was not present and was significantly lower than previously reported (p <0.001). A very slow rate of pressurizations (below Ipsi/minute) was associated with ear pain (OR = 3.32; 95% CI, 1.32-8.35; p <0.001).
Conclusion and Implications for Translation:
In this study, the AE reported in this prospective safety surveillance study are minor, and no objective barotrauma was reported. The HBOT at 1.45 ATA is a safe treatment that can be performed with a portable lighter and a less expensive hyperbaric chamber. This study supports the hypothesis that hyperbaric oxygenation therapy at 1.45 ATA is a safe treatment, allowing for the spread and application of adjuvant treatment in different pathologies.
Keywords
Safety
Portable
Hyperbaric Chamber
Oxygen Therapy
Adverse Events
Barotrauma
Introduction
Hyperbaric oxygen therapy (HBOT) is a treatment that uses hyperbaric chambers in order to increase environmental pressure.1 The patient breathes a high concentration of oxygen (usually near 100%) at a pressure higher than the atmospheric pressure.
Hyperbaric oxygen therapy has two indications: it can be used as an emergency treatment in certain acute pathologies in intensive care units or as outpatient therapy for long-term chronic pathologies. HBOT may be used to treat in carbon monoxide poisoning, gas embolism, necrotizing soft tissue infection, and decompression sickness. In some cases, it represents the primary treatment modality, whereas in others, it is an adjunct to conventional interventions.1 Guidelines are periodically updated and evaluated through consensus conferences. Several indications have been described, including off-label indications for rehabilitation, wellness, and aesthetic treatment.2 The occurrence of adverse events associated with HBOT is infrequent and typically not serious including otic/sinus barotrauma, confinement anxiety, hypoglycemia, oxygen toxicity, pneumothorax, seizure, and shortness of breath.3,4
Although nowadays it is performed at lower and safer pressures,5,6,7 there are some complications and side effects related to HBOT. Most safety studies are reported at pressures higher than 2 ATA.3,4.8,9 In general, HBOT is considered safe at pressures lower than 3 ATA when treatment sessions are less than 2 hours.4,10 However, pressure equalization problems in the middle ear, cranial sinus (sinus squeeze), and teeth (tooth squeeze) are common complications associated with HBOT. 11,12,13 It could be a factor of interrupting therapy, so the frequency of these and the population most susceptible to suffering should be studied.
Middle ear barotrauma (MEB) is one of the most common adverse events (AEs) of HBOT, with reported incidences ranging from 8% to 68.7% and up to 91% in patients unable to auto-inflate their middle ear.4,9 Patients may experience difficulty with ear equalization, a feeling of pressure, ear pain, and discomfort during the compression phase of HBOT.4
Ambiru et al. have reported that peripheral circulatory disorders with refractory ulcers or non-healing wounds and the interval between clinical symptoms and the first day of HBOT are independent risk factors for pressure equalization problems of the middle ear, the cranial sinus, and the teeth.14 This finding could be associated with peripheral circulatory disorders secondary to diabetes mellitus, which is an independent risk factor because almost all patients with this disease have diabetes mellitus.14 Other risk factors reported for MEB are repetitive treatments and pressure equalization problems.9 Some authors report no influence of age, gender, or mechanical ventilation on the occurrence of MEB,9 whereas one study found that age (≥ 61 years) and female gender are independent risk factors for cessation due to pressure equalization.14
Knowing before the first HBOT therapy session that patients are at high risk of complications of the therapy would make it possible to reduce the incidence of the complications by careful compression and decompression during HBOT. The rate of compression plays a role in MEB risk. It has been demonstrated that either a high rate of compression (4.1 psi/min) or a very slow rate of compression (<1 psi/min) increases the risk of MEB. It is possible that 2 psi/min is the best compression rate for minimizing MEB.4 In fact, a slower compression rate is often recommended to reduce the risk of symptomatic barotrauma,15 but a very slow rate is not recommended by other authors.4 Knowledge of the incidence of complications may contribute to patient counseling and may help to define the risk-benefit ratio in certain cases. Early recognition and appropriate management may also prevent complications and ensure that the patient could regulate the rate of compression in some portable hyperbaric chambers to prevent equalization complications when possible.
Although there have been numerous reports of the incidence of complications, no active surveillance study for pressures lower than 2 ATA has been reported.4,9,14 Almost all reported studies are based on retrospective studies, which could underdiagnose most of the minor events and incidences occurring during treatment.
Hadanny et al. have reported a retrospective analysis of the incidence of AE at different treatment pressures, finding a lower incidence of barotrauma at 1.5 ATA versus higher than 2 ATA,10 but this could be for indications that require lower pressure such as neurological indications.
The objective of this study is to analyze the safety of the treatment at 1.45 ATA using a portable hyperbaric chamber and compare it to the frequency reported at the same and higher pressures of treatment. Moreover, the secondary aim is to determine risk factors for equalization problems and the most adequate time to generate pressures lessening discomfort in patients receiving HBOT for different indications. A gap was discovered in the search for scientific bibliography for this trial, so it is anticipated that this trial will contribute to improving the scientific evidence.
Methods
This is a single-institutional active safety surveillance of AE. This prospective study included all the patients treated with HBOT at our facility from December 2019 to August 2021. Patients with no contraindications to treatment were included (pneumothorax, emphysema with carbon dioxide (CO2) retention, and, lung bullae).16
All participants provided written informed consent. Participants who were unable to provide consent to participate in this study were excluded. All procedures were conducted in accordance with the principles of the World Medical Association Declaration of Helsinki. The protocol was approved by independent ethics committees of participating healthcare centers. The study was carried out in compliance with Good Clinical Practice (GCP). The 6ethics committee of Servicio de Salud Metropolitano Oriente approved this study. Participants' personal data were protected and encrypted.
A minimum sample size of 89 patients was calculated based on a report of frequency of AE reported at 1.5 ATA (21.2%) and a minimum clinically relevant frequency of 8% in order to report the incidence and compare with AE had been yet reported by Hadanny et al.10 Standard statistical methods were used to calculate the mean and standard deviation (SD) or median with interquartile range as appropriate depending on distribution, and and the Shapiro-Wilk test was used to analyze the data. Binary variables are described in percentages with a 95% confidence interval (95% CI). Bivariate analysis was performed using Chi2 test, Fisher test, Student's t test, and paired t test, as appropriate. A p<0.05 was considered significant. Inferential analysis was performed using a bivariate analysis by calculating odds ratio (OR) with 95% confidence intervals; multiple logistic regression was used for multivariate analysis for different independent variables. A type I error of 5% and a type II error of 20% were set. Statistical analyses and sample size calculations were performed with Stata Version 13.0 (College Station, TX, USA).
HBOT consisted of 60-min sessions of hyperbaric oxygen therapy using Revitalair technology (fixed 1.45 ATA or 6.6 psi; Revitalair 430 ®, Oxavita SRL, Bs As, Argentina) pressurized with compressed air. Patients breathed an inspired fraction close to 100% of oxygen through reservoir masks. All adverse events were reported, including overall barotrauma, dizziness or weakness, dyspnea, claustrophobia or confinement anxiety, headache, hypoglycemia, sickness, chest pain, seizures, desaturation, and hypotension. Pre-and post--treatment otoscopy (graded using a modified Teed's scale),17 tympanometry, audiometry, and subjective ear complaints were recorded. The time to achieve a pressure of 1.45 ATA (6.6 psi) was reported as well as the rate of pressurization or depressurization for each session. Oxygen saturations (SpO2) were measured before and after the session using pulse oximetry (NONIN Onyx ® Vantage 9590). Basal supine blood pressure, heart rate (HR), and blood glucose level measurements were made before and after each session by medical team technicians. Blood pressure and HR were measured with the use of an electronic monitor (MedHouse, BP-2220). The Visual Analogue Scale18 was used to assess ear pain in patients, as well as the duration of the pain in each patient.
For the comparative analysis report, studies published from 2012 to 2021 in Medline, Embase, Breme, Lilacs, Scielo, and the Cochrane library were used. The medical subject heading (MeSH) terms used were hyperbaric oxygen therapy, safety, barotrauma, and adverse events. Furthermore, among published studies, information about AE at 1.5 ATA was searched to compare to our data.
For a general analysis of the indications and sessions of HBOT, each patient was assigned to one of four groups:
Group 1: Pain (fibromyalgia, chronic pain, neuropath-ic pain, arthritis, arthrosis);
Group 2: Wound (non-healing wounds, diabetic foot, non-neurological radiation injury, osteomyelitis, fractures);
Group 3: Rehabilitation (ischemic and hemorrhagic stroke, brain injury, facial palsy, brain injury tinnitus, post-COVID disease, Parkinson disease, and spinal cord injury);
Group 4: Prevention and wellness (wellness and anti-aging and pre-post surgery conditioning).
Prior to the first session, all patients were interviewed and examined. Chest X-ray was obtained from each patient with a history of pulmonary bullas or pneumothorax. History of epilepsy or seizures mandated a seizure-free interval of 6 months prior to treatment. Before each session, heart rate, blood pressure, and temperature were obtained in all patients, and blood glucose levels were measured in patients with diabetes. No patient with pneumothorax was accepted for treatment and relative contraindications included active bronchial asthma, severe obstructive pulmonary disease, and pregnancy. Patients with fever did not receive HBOT until their fever had subsided. HBOT was performed after obtaining written informed consent from each patient. Patients were informed about the risks of MEB and instructed to report any symptoms of ear pain or discomfort to the chaperone.
Results
In this study, we reported data from a single-institutional study of 175 patients who received 1,339 HBOT sessions in a portable monoplace hyperbaric chamber. The mean age was 52.9 ± 15.7 years; 98 (56%) were between 30 and 60 years. No children under the age of 16 years were treated in this period. The female-to-male ratio was 1.6:1 (Table 1). The number of HBOT treatments or sessions was 6 (3; 12) (median, 25th, and 75th percentile). The majority of patients received <10 sessions (65%), and the 55% had between 10 and 20 sessions of HBOT. Each session lasted 60 min. Only five patients (3%) had <60-min sessions (50-60 min). Pressurization and depressurization rates were 0.9 (0.7; 1.0) and 1.2 (1.0; 1.2), respectively (median; 25th and 75th percentile). The 62.4% of patients achieved over 6 min (<1 psi/min) during pressurization.
| Characteristic | N (%) |
|---|---|
| Age (years)a | 52.9±15.7 |
| Age (y) | |
| <30 | 15 (8.7) |
| 30-60 | 98 (56.7) |
| >60 | 60 (34.7) |
| Sex | |
| Male | 68 (38.9) |
| Female | 107 (61.1) |
| No. of HBOT treatmentsb | 6 (3; 12) |
| No. of HBOT treatments | |
| >20 | 4 (2.3) |
| 10-20 | 131.8 (55) |
| <10 | 114 (65.0) |
| Pressurization rate (psi/min)b | 0.86 (0.7;l.0) |
| Pressurization rate (min; psi/min), | N (%) |
| ≤6 min (≥1 psi/min) | 65 (37.6) |
| >6 min ≤10 min (≥0.6 <1 psi/min) | 96 (55.5) |
| >10 min (<0.6psi/min) | 12 (6.9) |
| Depressurization rate (p.s.i./min)b | 1.2 (l.0;l.2) |
| Depressurization rate (min; psi/min), n (%) | |
| ≤6 min (≥1 psi/min) | 118 (68.2) |
| >6 min ≤10 min (≥0.6 <1 psi/min) | 50 (28.9) |
| >10 min (<0.6psi/min) | 5 (2.9) |
| Pre-session saturation (%)b | 97 (97;99) |
| Post-session saturation (%)b | 99 (98;99)c |
| Pre-session heart rate (bpm)a | 77 (70;88) |
| Post-session heart rate (bpm)a | 74 (68; 82)c |
| Osteoarthritis/arthritis | 35 (20.2) |
| Pre-post surgery conditioning | 29 (16.8) |
| Fibromyalgia | 21 (12.1) |
| Refractory wound | 20 (11.6) |
| Wellness and anti-aging | 15 (8.7) |
| Chronic pain | 10 (5.8) |
| Post-stroke rehabilitation | 8 (4.6) |
| Parkinson disease | 8 (4.6) |
| Spinal cord injury | 5 (2.9) |
| Facial palsy | 5 (2.9) |
| Post-COVID rehabilitation | 5 (2.9) |
| Tinnitus | 3 (1.7) |
| Actinic cystitis | 3 (1.7) |
| Brain injury | 2 (1.2) |
| Others | 4 (2.3) |
aMean±SD; bMedian (25th percentile; 75th percentile), cp<0.001 between pre- and post-session values
Osteoarthritis (20.2%), surgery conditioning (16.8%), fibromyalgia (12.1%), and wounds (11.6%) were the most frequent indications for HBOT in this center.
Fifteen subjects (8.7) performed HBOT for wellness and anti-aging therapy. The indication that achieved more sessions in total was pain with 447 sessions for 66 patients (38% of the total; Table 2).
| Clinical Indications | Frequency (n, %) | Total Number of Sessions | Number of Sessionsa |
|---|---|---|---|
| Pain | 66 (38) | 447 | 8 (3;12) |
| Wound | 26 (15) | 349 | 8 (4;13) |
| Rehabilitation | 38 (22) | 397 | 9 (3;13) |
| Prevention and wellness | 43 (25) | 146 | 3 (2;9) |
| Total | 175 (100) | 1,339 | 6 (3;12) |
aMedian (25th percentile; 75th percentile)
The frequency and incidence of adverse events per session were 7.1% for total incidences and 4.1% for overall barotrauma. Of the total of 95 sessions with AE, 55(57.9%) presented subjective barotrauma, and 40 (42.1%) had non-barotrauma events (primarily dizziness/weakness for 10 patients). SpO2 was measured before and after each HBOT treatment session. Post-treatment SpO2 showed an immediate increase with median (25th and 75th percentile) 97 (97; 99) and 99 (98; 99) for pre- and post-treatment sessions, respectively (t =27.3; p <0.001; Figure 1a).
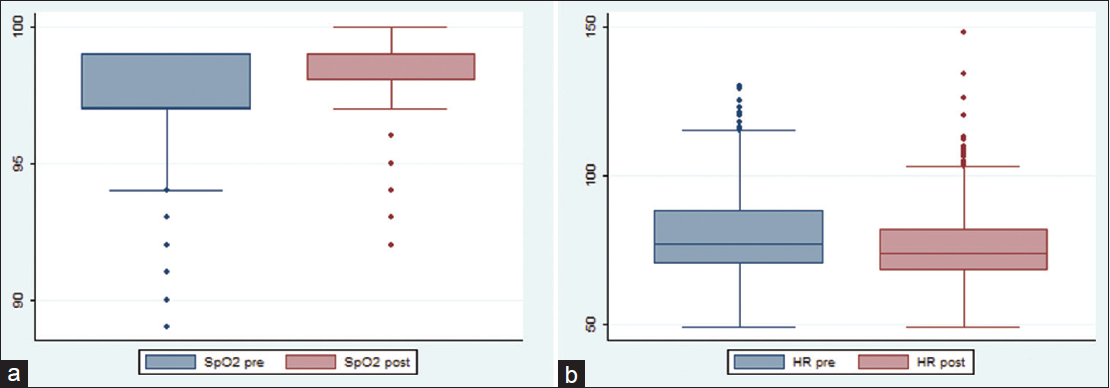
- Changes in oxygen saturation (SpO2, %) (1a) and heart rate (HR, bpm) (1b) before and after each session of HBOT
A reduction of heart rate after the HBOT session was recorded with a median of 77 (70;88) and 74 (68; 82) for pre- and post-session values, respectively (t= -12.1; p <0.001; Figure 1b). None of the patients presented hypotension in this study, and only one patient with diabetes reported hypoglycemia in two sessions.
Adverse events were reported in 28.3% of patients (n=49), with barotrauma and non-barotrauma AE in 20.3% (n=35) and 8.1% (n=14), respectively. All barotrauma was recorded as subjective (100% of ear ache without eardrum damage, Teed scale = 0).
Only one study was found reporting total AE in treatments performed at 1.5 ATA (Hadanny et al.). In our study, the frequency of total AE was statistically higher for 1.5, 2, and >2 ATA than in Hadanny et al. (Table 3). Non-barotrauma AE was also higher, but there was no objective barotrauma in our study, and it was significantly lower than previously reported (p <0.001, Table 4). Seizures and oxygen toxicity were not reported in our surveillance study. Ear pain was reported to have a median; 25th and 75th percentile duration of 2 min (1; 3) and a range of 10s to 60 min, with VAS scale values of 5.5 ±2.5 (mean± SD). Pressure equalization (discomfort without pain in the middle ear) was recorded in 20 patients (12.9%), with a duration of 2 (1; 3) min (median; 25th and 75th percentile) and intervals ranging from 10 s to 10 min. Cranial sinus pain (sinus squeeze) and tooth pain (tooth squeeze) were not observed in our study (Figure 2).
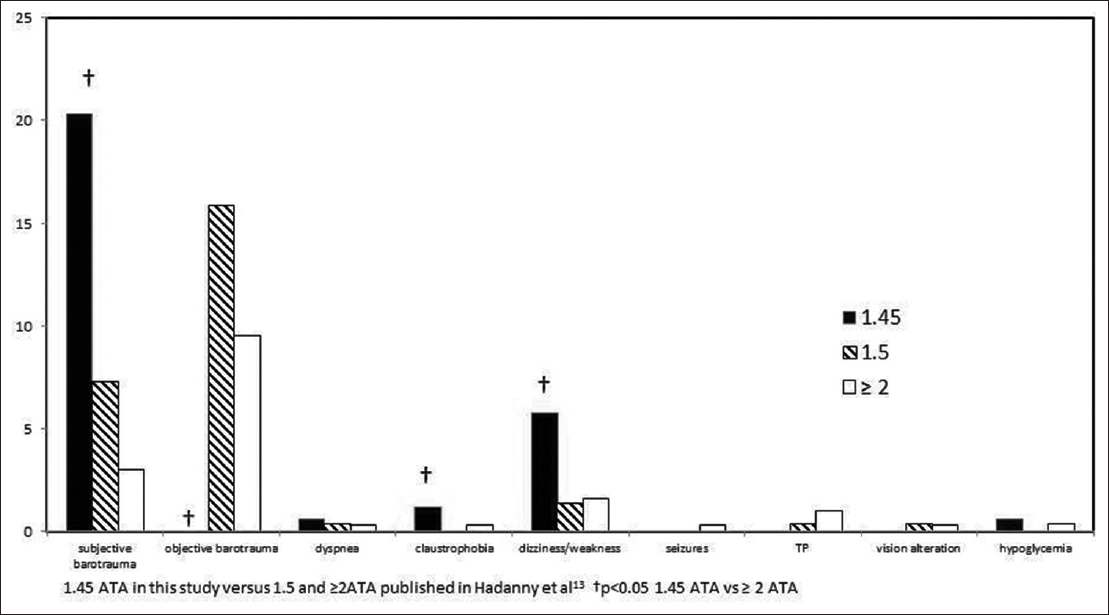
- Comparative frequencies of adverse events of hyperbaric oxygen therapy at different pressures of treatment
| Adverse Event | Sessions (n, %) |
|---|---|
| Subjective barotrauma | 55 (4.1) |
| Overall barotrauma | 55 (4.1) |
| Dizziness/weakness | 19 (1.4) |
| Dyspnea | 10 (0.7) |
| Claustrophobia | 7 (0.5) |
| Hypoglycemia | 2 (0.1) |
| Headache | 1 (<0.1) |
| Sickness | 1 (<0.1) |
| Chest pain | 0 (0.0) |
| Seizures | 0 (0.0) |
| Desaturation | 0 (0.0) |
| Hypotension | 0 (0.0) |
| Objective barotrauma | 0 (0.0) |
| Total non-barotrauma | 40 (2.9) |
| Total | 95 (7.1) |
| Adverse Events (AEs) or Complications | A (1.45 ATA) | B (1.5 ATA)b | p value A vs. B | C ≥ 2ATAb | p value A vs. C | D Totalb | p value A vs. D |
|---|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||||
| Subjective barotraumaa | 35 (20.3) | 16 (7.3) | <0.001 | 63 (3.0) | <0.001 | 79 (3.4) | <0.001 |
| Objective barotrauma | 0 (0.0) | 35 (15.9) | <0.001 | 196 (9.5) | <0.001 | 231 (9.9) | <0.001 |
| Total barotrauma | 35 (20.3) | 51 (25.2) | 0.148 | 259 (12.6) | 0.005 | 310 (13.3) | 0.005 |
| Dizziness/weakness | 10 (5.8) | 3 (1.4) | <0.001 | 33 (1.6) | <0.001 | 36 (1.5) | <0.001 |
| Claustrophobia | 2 (1.2) | 0 (0.0) | <0.001 | 6 (0.3) | 0.0395 | 6 (0.3) | 0.0395 |
| Dyspnea | 1 (0.6) | 1 (0.4) | 0.005 | 7 (0.3) | 0.504 | 5 (0.3) | 0.504 |
| Chest pain | 0 (0.0) | 1 (0.4) | 0.115 | 21 (1.0) | 0.186 | 22 (0.9) | 0.210 |
| Vision alteration | 0 (0.0) | 1 (0.4) | 0.115 | 7 (0.3) | 0.471 | 8 (0.3) | 0.471 |
| Hypoglycemia | 1 (0.6) | 0 (0,0) | <0.001 | 9 (0.4) | 0.710 | 9 (0.4) | 0.710 |
| Seizures | 0 (0.0) | 0 (0.0) | - | 7 (0.3) | 0.471 | 7 (0.2) | 0.556 |
| Total AE | 49 (28.3) | 57 (21.2) | 0.022 | 349 (16.9) | <0.001 | 406 (17.4) | <0.001 |
| Total AE non barotrauma | 14 (8.1) | 6 (2.2) | 90 (4.4) | 96 (4.1) | |||
| Equalization difficulty (without ear pain) | 64 (37.0) | N/R | - | N/R | - | N/R | - |
| Total | 175 | 271 | - | 2,063 | - | 2,334 | - |
aUnique or combined with dizziness, headache, and sickness; bValues recorded by Haddany et al.13; cComparison between A and B groups; dComparison between A and C groups; eComparison between A and D groups.
Using multivariate analyses, we examine other factors and assess their relationship to the complications to determine the significant independent risk factors of barotraumas and pressure equalization problems related to HBO2 therapy. Significantly higher middle-ear subjective barotrauma was noted when using the compression rate over 6 min (77.1% vs. 58.1%; p=0.04). After controlling for gender, age, general indications, number of sessions, and pressurization and depressurization time, there was an association between age (>60) and pressurization time of more than 6 min (OR: 2.28 and 3.32, p=0.032 and p<0.001, respectively) with ear ache (Table 5).
| Factors | Odds Ratio (95% CI) | p value | Probability (%) |
|---|---|---|---|
| For total pressure ear complications | |||
| Age (years) >60 | 2.01 (1.07-3.78) | 0.030 | 66.8 |
| Pressurization time duration >6 min (<1 psi/min) | 7.15 (3.17-16.10) | <0.001a | 87.7 |
| For ear ache | |||
| Age (years) > 60 | 2.28 (1.08-4.76) | 0.032 | 69.5 |
| Pressurization Time duration >6 min (<1 psi/min) | 3.32 (1.32-8.35) | <0.001a | 76.9 |
| For pressure ear equalization difficulties (without pain) | |||
| Pressurization time duration >6 min (<1 psi/min) | 8.32 (3.3-20.7) | <0.001a | 89.3 |
ap<0.001.
There was a significant association between the presence of equalization difficulty and ear ache (OR = 2.22; 95% CI, 1.00-4.88; Chi2 4.1; p=0.04). After controlling for the previously mentioned factors, the only risk factor for equalization difficulty (without pain) in this study was >6 min of pressurization time (<1 psi/min) (Table 5). Age >60 years had no significant association with the presence of pressure ear equalization difficult without pain OR = 1.47; 95% CI, 0.77-2.78; p=0.238). None of the patients were unable to continue HBOT therapy owing to severe pain due to pressure equalization difficulty, and none underwent myringotomy to continue HBOT.
Discussion
Hyperbaric oxygen therapy is an important adjunctive therapy in the treatment of chronic wounds, particularly those caused by late-effect radiation injury and diabetes, cyanide monoxide poisoning.16,19 The physiological effects and beneficial cellular response to oxidative stress required for tissue healing were reported using a portable hyperbaric chamber at pressures as low as 1.45 ATA in our study.20 In addition, the emergency use of portable- easy-to-use-lower-cost-lighter hyperbaric chambers for HBOT delivery would allow more patients to access treatments, resulting in an increase in off-label indications and wellness applications.
On the other hand, the hyperbaric chamber used in this study was demonstrated to be safe and efficient in hypoxemic patients with COVID-19.21 In this study, we report a significant increase in oxygen saturation with each session of HBOT as an efficient hyperoxia with a drop in heart rate in response to the hyperoxic and physiological vasoconstriction.22
Safety assessment is an essential skill to explore when a new medical device is incorporated as adjuvant therapy in each center. To the best of our knowledge, no active prospective surveillance of adverse events with similar portable hyperbaric chambers has been reported. There are no studies comparing rigid hyperbaric chambers with lighter ones with a focus on safety.
Hyperbaric oxygen therapy remains one of the safest therapies available today, with few reported side effects.3,4,10 In this study, we found a relatively low frequency of total AE, with MEB being the most common. The side effects described in this prospective surveillance study are self-limiting and often can be avoided with adequate screening. In addition, total AE could be overestimated (when compared with other studies) due to the researchers' active role in requesting minor AE, such as dizziness, weakness, or other discomforts in the patients receiving HBOT in this study.
Oxygen toxicity is rare at any pressure of treatment, and in this study, we did not record any signs of neurological or pulmonary toxicity. They are most commonly encountered as a central nervous system oxygen toxicity seizure that resolves with the withdrawal of oxygen and does not have any permanent implications. The probability of neurological oxygen toxicity or incidence of seizures is most likely reduced because of the protective action of lower pressures of treatment that do not induce neuro-excitability as much as higher ones.7 Furthermore, Hadanny et al.23 reported a lower incidence of seizures when 1.5 ATA was used, and some authors proposed pressures of treatment under 2 ATA for neurological indications as more effective and safer.24
Ocular side effects should be monitored. Hyperoxic myopia, which is one of the most common side effects, is considered reversible. One of the limitations of our study was that we did not monitor the degree of change during treatment to ensure safety, instead relying on the record of blurry vision after the HBOT session. This can be done by driving and instructing them to keep track of their progress until at least 8 weeks after treatment is completed. 25 However, using a reservoir mask instead of a hood or an oxygen-enriched atmosphere inside the chambers reduces the risk of visual changes as AE.26
Hypoglycemia during HBOT is a common concern, and it is clinically relevant,4 but it is not common. In this study, we only recorded one patient with diabetes who had two episodes of hypoglycemia after the session. Further studies and active surveillance should be performed using test strips in selected populations, particularly insulin-dependent ones.
Claustrophobia may be managed with coaching and anxiolytic medications. Intolerance of a monoplace chamber may warrant referral to the nearest multiplace chamber facility.4 This must be considered when comparative studies are performed. We recorded higher anxiety confinement at 1.5 ATA when compared with the other report, but this is likely due to the type of hyperbaric chamber used in Haddany et al.10 However, the innovative design of the hyperbaric chamber used in our study (10 transparent windows around the device) allows claustrophobia to be considered as relative instead of absolute contraindication. More preventive strategies and professional accompaniment could be used to allow patients with a history of claustrophobia not to interrupt HBOT sessions. In our study, the two patients who reported claustrophobia were able to complete the treatment.
However, one of the most common side effects related to pressure changes is MEB. Although it is common, it is typically mild and self-limiting. MEB is one of the most common side effects of HBOT. Patients may report difficulty with ear equalization, a sense of pressure, ear pain, and discomfort during compression.4
In this study, subjective barotrauma (ear pain or otalgia) has been reported in higher frequency than in Hadanny et al. However, in the study performed by Hadanny et al. (the only safety study that reported treatment at 1.5 ATA after a systematic search), ventilation tube insertion or myringotomy was performed before treatment initiation in 79 patients (3.4%), and these patients were excluded from the study.10 This could reduce the incidence of total barotrauma.
Importantly, there was no objective barotrauma (ear ache without objective signs of MEB per otoscopy) in our study. Otological complications and MEB were present in almost all safety studies of different hyperbaric chambers (8.9-66.7).11 Hadanny et al. reported 15.9% objective barotrauma in patients receiving HBOT at 1.5 ATA (excluding patients with myringotomy).10
Middle ear barotrauma can be transmitted to the inner ear, causing rupture of the round or oval window membranes and impairment of inner ear function, resulting in vertigo and sensorineural hearing loss.4,15 Many studies, with a focus on barotrauma, report potential risk factors associated with HBOT complications.8,14,15 The rate of compression does play a role in the risk of MEB. According to a 2017 study, either a high rate of compression (4.1 psi/ min) or a very slow rate of compression (1 psi/min) increased the risk of MEB.4 However, a slow rate of compression was not significantly associated with a reduction of MEB (48% vs. 29%, p=0.02).15
In our study, a very slow rate of pressurizations (below 1psi/min) was significantly associated with otological complications, pressure-equalizing problems without pain, and ear pain. It is not clear to us if it could be a risk factor or a consequence because of the advantage of the hyperbaric chamber to self-regulate the rate of pressurization using a control set inside the chamber. Perhaps equalization problems made patients with an anatomical predisposition to MEB to reduce their own rate of pressurization.
Importantly, the absence of eardrum damage or Teed scale > 0 in our study was significantly lower than other studies performed at 1.5 or higher pressures of treatment.3,8,10,14 Only ear pain without damage and discomfort were reported at a higher proportion than in other studies, but this could be due to the study design (active surveillance prospective cohort).
There is an increased risk of MEB during initial treatments, but no increased risk is associated with a longer treatment course reported in other studies.9,14,15 A limitation of our study was the low number of repetitive treatments (below 20). However, it could be related to the type of indications, and repetitive treatments were reported as a risk factor, most likely due to the presence of monoxide carbon poisoning, which requires less than five treatment sessions.9
Ambiru et al.14 reported that the presence of barotrauma to peripheral circulatory disorders with refractory ulcers or non-healing wounds and the interval between clinical symptoms and the first day of HBOT were independent risk factors of pressure equalization problems of the middle ear, the cranial sinus, and the teeth. Besides, another study confirmed that significant risks could be age, female, and different indications, such as radiation injuries, hearing loss, and carbon monoxide poisoning.11 Although our study has included patients with refractory wounds and radiation injuries, we found no influence of the type of indication in otological alterations.
Age is a controversial risk factor because of the contradictory results in several studies.8,9,14 We found an association between age > 60 years and ear pain, but in our study, we did not report objective barotrauma. Yamamoto et al.8 reported that 14.8% of patients had ontological symptoms and 50% of those patients had Teed scale > 0 and reported an association between age and MEB. Other researchers reported age as a risk factor for cessation due to pressure equalization problems.16 However, no cessation was reported among patients receiving HBOT in this period in our study.
It is important to consider that Eustachian tube function deterioration is associated with age and anatomical characteristics.27 An important limitation is that this surveillance study does not include any pediatric patients.
An important association of equalizing problems (without pain) and ear ache is reported6 in this study but some variables reported as risk factor of Eustachian tube obstruction (such as rhinitis or anatomical dysfunction) have been recorded in our study. It is important to continue reporting the presence of rhinitis and to include the pediatric population in the surveillance. An evaluation of the Eustachian tube function starting the first session of HBOT could be a good predictor of future otological complications.
Difficulties with equalizing pressure were associated with MBE in other studies,8,9,14 whereas patients who did or did not perform a Valsalva had the same MEB incidence in some studies.15 This could be explained by a number of patients performing ineffective Valsalva, who would be at a higher risk for MEB. On the other hand, Lima et al.28 demonstrated that positive Valsalva (with good insufflation before the first session alone or associated with Toynbee maneuvers) was a protective factor for MEB after the first session. Furthermore, the Eustachian tube function test could be the primary predictor of MEB29 in a variety of patients receiving HBOT A randomized clinical trial is currently being conducted to evaluate the effect of self-acupressure on MEB as an adjuvant to the Valsalva and Toynbee maneuvers.30
Meanwhile, our study has demonstrated that performing HBOT at 1.45ATA in a portable lighter hyperbaric chamber could be safer than reporting in another chamber. It has been demonstrated that hyperoxia is caused by increasing oxygen saturation in the blood. All of the AEs reported in this safety surveillance study were minor, and no objective barotrauma was reported. None of the patients were unable to continue HBOT therapy owing to severe pain due to pressure equalization difficulty, and none underwent myringotomy to continue HBOT. This team presented weaknesses in the development of the trial. It was not possible to evaluate the anatomical conditions of the patients or other risk factors, so we cannot affirm that they are or are not related to the results.
Although it was not recorded, applying training in different maneuvers in order to prevent otological complications and adjustment of the treatment protocol to decrease the incidence of ear pain were an actual challenge for us. It is a priority to establish and discover these complications in order to improve the comfort of the patients during HBOT. This will be extrapolated to centers that used portable hyperbaric chambers, demonstrating safety in new paradigms for performing HBOT as advantages for expanding clinical applications of this treatment.
Conclusion and Implications for Translation
Hyperbaric oxygen therapy at 1.45 ATA performed in a portable lighter hyperbaric chamber could be safer than reporting in other chambers. It has been demonstrated that hyperoxia is produced by increasing oxygen saturation in the blood with a physiological reduction of heart rate. AE per session was 7.1% for totalAE and 4.1% for overall barotrauma. All of the AEs reported in this safety surveillance study were minor, and no objective barotrauma was reported. HBOT at 1.45 ATA is a safe treatment that can be performed with a portable lighter and a less expensive hyperbaric chamber.
Compliance with Ethical Standards
Conflicts of Interest:
The authors declare no competing interests.
Financial Disclosure:
Nothing to declare.
Ethics Approval:
Ethics committee of Servicio de Salud Metropolitano Oriente approved this study. Santiago, Chile
Disclaimer:
None.
Acknowledgments:
The authors would like to thank Liliana Jorda-Vargas, for their contribution to the development and publication of this manuscript.
Funding/Support:
There was no funding for this study.
References
- Hyperbaric oxygen therapy in Plastic Surgery practice: case series and literature overview. G Chir. 2019;40(4):257-275.
- [Google Scholar]
- A retrospective analysis of adverse events in hyperbaric oxygen therapy (2012-2015): lessons learned from 1.5 million treatments. Adv SkinWound Care. 2017;30(3):125-129.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperbaric oxygen therapy: side effects defined and quantified. Adv Wound Care. 2017;6(6):210-224. (New Rochelle)
- [CrossRef] [PubMed] [Google Scholar]
- Reflections on the neurotherapeutic effects of hyperbaric oxygen. Expert Rev Neurother. 2014;14(3):233-236.
- [CrossRef] [PubMed] [Google Scholar]
- Intensive rehabilitation combined with HBO2 therapy in children with cerebral palsy: a controlled longitudinal study. Undersea Hyperb Med. 2014;41(2):77-85.
- [Google Scholar]
- Effect of oxygen on neuronal excitability measured by critical flicker fusion frequency is dose dependent. J Clin Exp Neuropsychol. 2015;37(3):276-284.
- [CrossRef] [PubMed] [Google Scholar]
- Otological complications associated with hyperbaric oxygen therapy. Eur Arch Otorhinolaryngol. 2016;273(9):2487-2493.
- [CrossRef] [PubMed] [Google Scholar]
- Middle-ear barotrauma after hyperbaric oxygen therapy. Undersea Hyperb Med. 2010;37(4):203-208.
- [Google Scholar]
- The safety of hyperbaric oxygen treatment--retrospective analysis in 2,334 patients. Undersea Hyperb Med. 2016;43(2):113-122.
- [Google Scholar]
- Middle ear barotrauma during hyperbaric oxygen therapy; a review of occurrences in 5,962 patients. Undersea Hyperb Med. 2019;46(2):101-106.
- [CrossRef] [PubMed] [Google Scholar]
- Inner and middle ear hyperbaric oxygen-induced barotrauma. Laryngoscope. 1997;107(10):1350-1356.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective analysis of independent patient risk factors for middle ear barotrauma in a multiplace hyperbaric chamber. Diving Hyperb Med. 2013;43(3):143-147.
- [Google Scholar]
- Analysis of risk factors associated with complications of hyperbaric oxygen therapy. J Crit Care. 2008;23(3):295-300.
- [CrossRef] [PubMed] [Google Scholar]
- Does the slow compression technique of hyperbaric oxygen therapy decrease the incidence of middle- ear barotrauma? J Laryngol Otol. 2006;120(6):446-449.
- [CrossRef] [PubMed] [Google Scholar]
- Textbook of Hyperbaric Medicine 2017
- [CrossRef]
- The Visual Analogue Scale for Rating, Ranking and Paired-Comparison (VAS-RRP): A new technique for psychological measurement. Behav Res Methods. 2018;50(4):1694-1715.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperbaric oxygen: its mechanisms and efficacy. Plast Reconstr Surg. 2011;127(Suppl 1 (Suppl 1)):131S-141S.
- [CrossRef] [PubMed] [Google Scholar]
- Increasing oxygen partial pressures induce a distinct transcriptional response in human PBMC: a pilot study on the “Normobaric Oxygen Paradox.”. Int J Mol sci. 2021;22(1):458.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperbaric oxygen as an adjuvant treatment for patients with COVID-19 severe hypoxaemia: a randomised controlled trial. Emerg Med J. 2022;39(2):88-93.
- [CrossRef] [PubMed] [Google Scholar]
- Influences of hyperbaric oxygen on blood pressure, heart rate and blood glucose levels in patients with diabetes mellitus and hypertension. Arch Med Res. 2006;37(8):991-997.
- [CrossRef] [PubMed] [Google Scholar]
- Seizures during hyperbaric oxygen therapy: retrospective analysis of 62,614 treatment sessions. Undersea Hyperb Med. 2016;43(1):21-28.
- [Google Scholar]
- A phase I study of low-pressure hyperbaric oxygen therapy for blast-induced post-concussion syndrome and post-traumatic stress disorder. J Neurotrauma. 2012;29(1):168-185.
- [CrossRef] [PubMed] [Google Scholar]
- McMonnies CW Hyperbaric oxygen therapy and the possibility of ocular complications or contraindications. Clin Exp Optom. 2015;98(2):122-125.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular refractive changes in patients receiving hyperbaric oxygen administered by oronasal mask or hood. Acta Ophthalmol Scand. 2004;82(4):449-53.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in eustachian tube function with age in children with normal ears. A longitudinal study. Acta Otolaryngol. 1983;96(5-6):467-477.
- [CrossRef] [PubMed] [Google Scholar]
- Middle ear barotrauma after hyperbaric oxygen therapy - the role of insuflation maneuvers. Int Tinnitus J. 2012;17(2):180-185.
- [CrossRef] [PubMed] [Google Scholar]
- Eustachian tube function test as a predictor of middle ear barotrauma. Int Marit Health. 2020;71(3):195-200.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of self--acupressure on middle ear barotrauma associated with hyperbaric oxygen therapy: A nonrandomized clinical trial. Medicine (Baltimore). 2021;100(17):e25674.
- [CrossRef] [PubMed] [Google Scholar]





