Translate this page into:
Improving Reproductive and Maternal Healthcare Uptake in India: An Evaluation of Project Ujjwal Public-Private Partnership Program
✉Corresponding author email: anagha_lokhande@brown.edu
Abstract
Background and Objective:
Project Ujjwall was a public private partnership established to improve maternal and child health (MCH) outcomes in Bihar and Odisha in India. This paper examines whether Project Ujjwal meaningfully increased the usage of family planning methods and maternal health services to determine whether the Ujjwall program model should be expanded in India. This is the first attempt to establish the causal impact of Project Ujjwal on access to reproductive healthcare in India.
Methods:
Data were obtained from the National Family Health Survey of India. A difference-in-differences strategy and linear probability models were used to estimate the likelihood of ever having encountered family planning information or ever having used contraceptives, antenatal care, etc.
Results:
The sample size for Odisha was 4,540; the sample size for Bihar was 3,818; the total sample size for all states in the control group was 24,922. Within Odisha and Bihar, Project Ujjwal increased the likelihood of ever having used any contraceptive by 8.9%, increased the likelihood of having ever accessed antenatal care from a licensed doctor or nurse by 2.5% and increased the likelihood of having ever encountered family planning media by 5.1%. However, most results seem differentially driven by the success of the program in either Odisha or Bihar: among all results, only the odds that a woman received delivery assistance (2.8%) and the odds that a woman will have used oral contraceptives by (9.3%) increased statistically significant in both states.
Conclusion and Implications for Translation:
These results are promising and show Project Ujjwal may have been more effective than existing government programs. Limitations of this analysis include a lack of information about the demand generation tactics and an inability to include state-level fixed effects due to over-specification concerns. Disparities in the impact of Project Ujjwal on Bihar and Odisha and the lack of specific information about latent demand both suggest the need for further investigation.
Keywords
Reproductive Health
Maternal Health
Child Health
India
Policy Evaluation
Difference-in-Differences
1. Introduction
1.1. Background of the Study
Family planning has been shown to have a profound impact on women's educational attainment and labor force participation.1 Ascertaining the effectiveness of reproductive health interventions can help design future programs. In particular, determining which features of a program or target population drive program success can aid policymakers in emulating and appropriately adapting successful programs.2
There is a robust body of literature investigating the effects of various family planning interventions in low- and middle-income countries. Prior work on supply-side interventions has demonstrated that in the absence of modern contraceptive methods, fertility control can be costly and infeasible as it often requires women to forgo desired sexual activity or negotiate sexual activity and fertility with men, who have much greater bargaining power.3 Prior evidence from demand-side interventions demonstrated decreases in fertility rates and infant mortality, and increased female labor force participation.1 Further work has demonstrated that network effects4 and healthcare appointments without a male spouse present may play an important role in female contraceptive adoption.5
India's National Health Mission has aimed to improve maternal and child health through several programs. Established in 1975, Anganwadi Centers are community health centers that aim to provide prenatal care and contraceptive counseling and supplies. However, workers in Anganwadi Centers often earn low wages and the centers themselves have been plagued with charges of corruption and inefficiency.6 As a supplement to Anganwadi Centers, the federal government of India instituted Accredited Social Health Activists (ASHAs), government community health workers tasked with assisting Anganwadi centers and performing outreach efforts. Unfortunately, there is mixed evidence on the efficacy of ASHAs; prior work has demonstrated that multitasking problems caused by their myriad responsibilities may inhibit their ability to meaningfully improve health inputs.7 In 2006, the Indian federal government created the Janani Suraksha Yojana, a conditional cash transfer program that paid women for giving birth in hospitals as opposed to in their homes. This program was shown to reduce overall maternal mortality but failed at targeting the poorest and highest risk women.8
Project Ujjwal was a public-private partnership between the Palladium Group (an international advisory company), the Hindustan Latex Family Planning Promotion Trust (a non-profit condom manufacturer), the Johns Hopkins School of Public Health, and the Governments of Bihar and Odisha. The project ran from 2013 through 2016 in the Indian states of Odisha and Bihar, two of the least developed states in the country.9,10 These states also both perform poorly in state-wise rankings of gender equality: as compared to their male counterparts, women in these states have been shown to experience significantly lower health, employment, and education levels.11
Project Ujjwal differed from many other programs in India with similar goals in that these other programs are primarily federal programs run by the government of India and involve neither private sector advising at administrative level nor private sector participation at the service delivery level.12
The program's goals were to: (a) increase access to reproductive care and improve maternal and child health outcomes and (b) create sustainable revenue streams for providers of reproductive products and services. The latter goal is another differentiating factor between Ujjwal and existing federal programs such as Anganwadi centers that pay workers a fixed salary. As discussed below, Ujjwal facilitated reimbursement of private health clinics on a per- procedure basis and paid micro-franchisees on a per-referral or per-sale basis. The program sought to augment both supply and demand for family planning products and services, with the Palladium Group and the Hindustan Latex Family Planning Promotion Trust coordinating the supply operations and Johns Hopkins coordinating the demand operations.12
Supply was expanded through the development of a three-tier fractional franchise model in which potential franchisees are already part of the same line of business as the franchiser (joining the franchise is an add-on to the franchisee's existing business). Tier 1 of the model involved contracting existing medium sized private clinics to offer a full range of family planning services including antenatal and postnatal care and abortions. Tier 2 of the model involved contracting smaller, rural clinics to provide a more narrow range of these services (e.g. Tier 1 clinics provided first and second trimester abortions and tubal ligation while Tier 2 clinics provided only first trimester abortions and non-permanent contraceptive methods).12
All services were provided free of charge. Ujjwal facilitated the accreditation of private providers for government reimbursements through the National Health Mission in India. The project also facilitated provider empanelment for insurance schemes through a large means-tested government insurance program (Rashtriya Swasthya Bima Yojana).12
Tier 3 of the model was the hiring of Ujjwal Saathis, community-based entrepreneurs (microfranchisees) who promoted Project Ujjwal clinics and provided contraceptive outreach, screening and counseling to prospective clients while also dispensing and selling products. Each Ujjwal clinic was linked to 15-20 Ujjwal Saathis, 8-10 of whom tended to be most active. Saathis received a fee from clinics for referring patients and averaged six referrals per month across both states. The sale of products was a secondary source of income. Consistent with the fractional franchise model wherein franchisee are already in the same line of business as the franchiser, ASHAs were eligible to become Ujjwal Saathis and receive additional income through their involvement with the project. Ujjwal Saathis were almost exclusively women and were available to meet with female community members privately or with community members and their partners.12
Though Tier 3 of the supply model worked to bolster demand in addition to supply, Ujjwal also included a separate demand generation campaign, targeted toward couples (as opposed to only toward women), that included a mass media campaign and attempts to increase community engagement with the program. This included over 5,000 street theater shows, a mobile application, television and radio advertisement campaigns, and posters and billboards advertising the project.12
1.2. Objectives of the Study
This study is the first examination of the impact of Project Ujjwal on improving reproductive and maternal healthcare uptake in Odisha and Bihar. Given Project Ujjwal's novel structure, it may be especially difficult for policymakers to gauge the program's impact and the applicability of its format to other settings. Quantitatively assessing Project Ujjwal's effectiveness may provide policymakers with preliminary insight into whether a public-private partnership and combined supply- and demandgenerating structure may be viable for further use.
1.3. Specific Aims and Hypothesis
A difference-in-differences empirical framework was used to assess whether reproductive and maternal healthcare uptake increased in Odisha and Bihar at a greater rate than in their neighboring states following the introduction of Project Ujjwal. Prior evidence from South Asia has demonstrated that multilayered community-based interventions improve utilization of reproductive healthcare.13 Given that Project Ujjwal follows a similar structure as prior successful interventions, one may hypothesize that it would be similarly successful. The analysis herein seeks to ascertain whether that is the case.
2. Methods
At the time of this study, there is no publicly available data specifically measuring Project Ujjwal's impact. Accordingly, all data used in this study were from the National Family Health Survey (NFHS) of India, a comprehensive countrywide dataset that includes a variety of survey variables measuring family and individual health factors. Individual-level data for female survey respondents were used. All four rounds of the survey were used in this analysis: 1992-1993 (NFHS-1), 1998-1999 (NFHS-2), 2005-2006 (NFHS-3), and 2015-2016 (NFHS-4).14 Data were accessed through the Demographic and Health Surveys (DHS) Program and harmonized across years using DHS recode manuals.15
In 2000, regions of different three states in India became their own states: Bihar split into Bihar and Jharkhand; Uttar Pradesh split into Uttar Pradesh and Uttarakhand; Madhya Pradesh split into Madhya Pradesh and Chhattisgarh. In this analysis, Bihar is in the treatment group while Jharkhand is in the control group; Uttar Pradesh is in the control group while Uttarakhand is excluded, and both Madhya Pradesh and Chhattisgarh are in the control group. To standardize treatment and control groups for all years of the analysis, district level data from NFHS and the Indian census were used. Districts that remained in the original states were separated from those that became part of the new states.14-16
2.1. Study Variables
Contraceptive usage, antenatal care, and delivery assistance were selected as outcome variables because these were all measures explicitly targeted by the program. However, also included is an input that attempts to capture some of the effects of the demand-side effort: likelihood of having encountered information about family planning through media (television, radio, or billboard), as a proxy for demand generation: women who are unaware of available family planning options are less likely to desire access to those resources and vice versa.17
2.2. Statistical Analysis
State-by-year difference-in-difference regressions of the following form were employed:
γst= ɑ + β. I{s = treat}. I{t ≥ 2015} + γt+ X'stδ + εst
The variable γst is the outcome of interest for s in year t. The coefficient of interest is β, which represents the difference-in-difference estimate of the effect of Project Ujjwal. This coefficient is identified by (a) comparing outcomes for Bihar/ Odisha and the control states and (b) comparing outcomes in Bihar/Odisha before and after the program. The first indicator variable, I{s = treat} identifies the former. In this paper, the effect of the program in Bihar, the effect in Odisha, and the total effect are estimated. Therefore, the definition of the treatment group varies throughout the course of this paper and this indicator variable should be interpreted accordingly. When estimating the total impact of the program, the indicator takes on a nonzero value for observations from either Bihar or Odisha. When estimating the impact of the program in Odisha, the indicator takes on a nonzero value only for observations from Odisha or only for those from Bihar. When running the latter two regressions, the other treatment state was omitted from the sample, i.e., when estimating the impact of the program in Odisha, observations from Bihar were removed from the sample.
The second indicator variable I{t ≥ 2015} identifies the difference in outcomes between the pre- and post-treatment periods, i.e., after 2014. The model also includes year fixed effects (γt) and a vector of time-varying controls measured at the state level (X'stδ). State fixed could not be used: since the number of states being used is so small, the inclusion of state fixed effects causes the model to become overdetermined and leads to multicollinearity issues. State trends are therefore included as part X' stδ. The error term is εst which is assumed to be uncorrelated with other unobserved determinants of the outcome variable.
The identification assumption made in this model is the parallel trends assumption: outcomes in Bihar and Odisha would not have evolved differently from the control states in the absence of the treatment. States in the control group are therefore those which are geographically proximate and socioeconomically similar to Bihar and Odisha. Bihar and Odisha are both considered northern states; north and south India differ dramatically in terms of politics, demography, climate, etc.18 Removing southern states eliminates some concern about unobservable error. To rigorously create the control group from the remaining states, t-tests were used to compare education and income levels of the two treatment states and remaining possible control states. The parallel trends assumption was then assessed graphically by plotting pre-treatment trends in the control and the treatment groups.
Due to the limitations in available data, a linear probability model that investigates binary outcomes was used. Binary outcomes were the only relevant outcomes consistently available across all survey years. Results can therefore be interpreted as a change in the likelihood that a given woman in the treatment group has ever used an intrauterine device (IUD), ever heard about family planning through media, etc. Because this model explicitly violates the ordinary least squares (OLS) homoscedasticity assumption, because observations are clustered at the state level wherein errors are serially correlated, and because only using a small number of states are used, a standard bootstrap method repeated 100 times was used to calculate standard errors. All analyses were conducted in Stata.19
2.3. Ethical Approval
The institutional review board of Brown University, United States determined that the research activities did not include human subjects because they are based on secondary analysis of deidentified data sources.
3. Results
3.1. Sociodemographic Characteristics
Table 1 summarizes key statistics for these states and others in northeastern India. These statistics are consistent with work in northeast India and show that relative to their neighbors, Odisha and Bihar have lower education rates and income levels, and higher levels of unmet family planning needs. The sample size for Odisha was 4,540; the sample size for Bihar was 3,818; the total sample size for all states in the control group was 24,922.
| Unmet Spacing Need (1) | Unmet Limiting Need (2) | Income (3) | Education (4) | |
|---|---|---|---|---|
| Bihar | 10.6 | 12.1 | -70461 | 2.06 |
| Odisha | 6.8 | 8.1 | -61930 | 2.75 |
| Assam | 3.3 | 7.0 | -51393 | 3.11 |
| Chhattisgarh | 5.1 | 4.7 | -42004 | 2.22 |
| Jharkhand | 11.3 | 11.8 | -56300 | 2.62 |
| Madhya Pradesh | 5.4 | 5.9 | -40030 | 2.83 |
| Meghalaya | 23.2 | 11.8 | -24027 | 3.48 |
| Sikkim | 5.6 | 11.1 | 32272 | 4.03 |
| Uttar Pradesh | 8.8 | 11.1 | -28708 | 2.66 |
| West Bengal | 3.5 | 3.9 | -52060 | 3.13 |
Column (1) shows the percentage of women in each state who have unmet need for family planning products/services to space births. Column (2) shows the percentage of women in each state who have unmet need for family planning products/services in order to limit births. Column (3) shows income as measured by a computed wealth index from the dataset. Column (4) shows average years of completed education for women. All data is from the 2005-2006 NFHS.
3.2. Main Variable (Dependent or Outcome) Results
Table 2 shows a summary of the results. Project Ujjwal apparently increased the likelihood of ever having used any contraceptive by 8.9%, increased the likelihood of having ever accessed antenatal care (from a licensed doctor or nurse) 2.5%, increased the likelihood of having ever received assistance with delivery (by a licensed doctor or nurse) by 2.8%, and increased the likelihood of having ever encountered family planning media by 5.1%. A graph of the percentage of women who have ever used contraception, in both the pre- and post-intervention period, is shown in Supplementary Figure 1. These findings are deferentially driven by success in either Bihar or Odisha; only delivery assistance appeared to increase in both states.
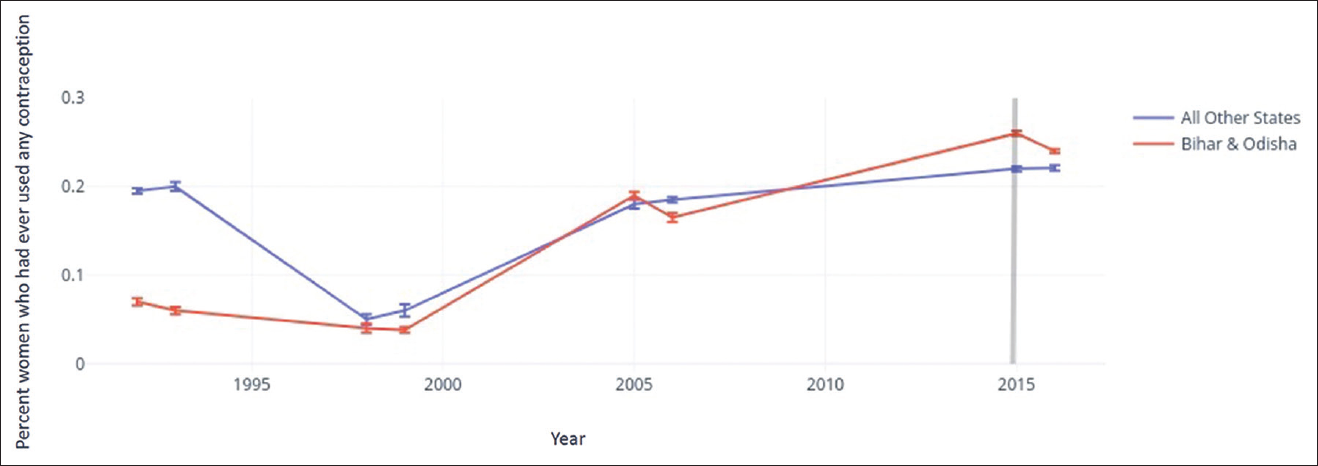
- The percentage of women who had ever used contraception. The grey line represents the fìrst available data after the onset of the intervention, i.e., NFHS-4 data
| Contraceptive Usage (1) | Antenatal Care (2) | Delivery Assistance (3) | Encountered FP Media (4) | |
|---|---|---|---|---|
| Treat x post | 0.089*** (0.011) | 0.025*** (0.003) | 0.028*** (0.003) | 0.051*** (0.003) |
| Bihar x post | 0.089*** (0.014) | 0.059*** (0.004) | 0.063*** (0.004) | -0.012*** (0.005) |
| Odisha x post | 0.005 (0.022) | -0.001*** (0.004) | 0.008** (0.003) | 0.081*** (0.005) |
This table shows the impact of Project Ujjwal on the listed health inputs. Column (1) shows the impact of the project on the likelihood of ever having used any kind of contraceptive. Column (2) shows its impact on the likelihood of ever having accessed antenatal care from a licensed doctor or nurse. Column (3) shows its impact on the likelihood having ever received delivery assistance from a licensed doctor or nurse. Column (4) shows its impact on the likelihood of having encountered family planning resources on the radio, on a billboard, or on television. Treat represents the combined values for Bihar and Odisha, while the second and third rows show results for each state individually. *Significance at the 10% level. ** Significance at the 5% level. *** Significance at the 1% level.
3.3. Results of Other Variables
Table 3 shows results for general contraceptive usage based on contraceptive type. There was a 9.3% increase in likelihood of having ever used a birth control pill. All other results are either statistically insignificant or different between Bihar and Odisha, though likelihood of ever having used an injectable contraceptive did not change in any statistically significant way in either state or overall.
| Pill (1) | Injection (2) | IUD (3) | Tubal Ligation (4) | Condom (5) | Vasectomy (6) | |
|---|---|---|---|---|---|---|
| Treat x post | 0.093*** (0.002) | 0.0002 (0.001) | 0.009*** (0.002) | 0.001 (0.004) | 0.030*** (0.004) | -0.034*** (0.003) |
| Bihar x post | 0.028*** (0.003) | 0.001 (0.002) | 0.041*** (0.002) | -0.082*** (0.005) | 0.124*** (0.004) | 0.040*** (0.003) |
| Odisha x post | 0.133*** (0.005) | -0.001 (0.001) | -0.020*** (0.003) | 0.060*** (0.005) | -0.042*** (0.005) | -0.088*** (0.003) |
This table shows the breakdown of Project Ujjwal's impact on contraception usage. Column (1) shows the impact of the project on the likelihood of ever having used birth control pills. Column (2) shows its impact on the likelihood of ever having used injectable contraceptives. Column (3) shows its impact on the likelihood having ever used an intrauterine device (IUD). Column (4) shows its impact on the likelihood of having received a tubal ligation (female sterilization). Column (5) shows its impact on the likelihood of partner having ever used a condom. Column (6) shows its impact on the likelihood of partner having had a vasectomy Treat represents the combined values for Bihar and Odisha, while the second and third rows show results for each state individually * Significance at the 10% level. ** Significance at the 5% level. *** Significance at the 1% levels
The likelihood of exposure to family planning information via media was measured to approximate the effectiveness of demand generation. The likelihood of this exposure increased by 5.1% overall, having increased in Odisha and decreased in Bihar. However, likelihood of any type of contraceptive usage increased in Bihar and likelihood of any type of contraceptive usage did not change in Odisha. There are also increases in likelihood of having used certain types of contraceptives, but these differ by state.This suggests that in the context of Project Ujjwal, mere exposure to family planning information via media is not correlated with any changes in the probability of contraception use.
4. Discussion
Project Ujjwal's most significant impact was an apparent 8.9% increase in likelihood of having ever used contraception across both states. This was perhaps driven by the large increase (13.3%) in the likelihood of having ever used birth control pills in Odisha. A second significant impact was the 2.8% increase in the probability that a woman received delivery assistance from a licensed doctor or nurse. Delivery assistance was the only variable investigated in which Project Ujjwal appeared to have an impact in both states. Changes in the other variables were inconsistent across both states.
4.1. Strengths and Limitations of the Study
To date, this is the first attempt at empirically assessing Project Ujjwal's impact. The findings herein are consistent with prior work on the efficacy of multi-layered community-based interventions for reproductive healthcare uptake in South Asia.13
However, this work has some limitations. State- level fixed effects were excluded as their inclusion led to over-specification of the model; it is possible that these two states differed in some unobserved way that caused inconsistencies in program impact. Additionally, the likelihood of exposure to family planning materials via media outcome inadequately captures the full effect of Project Ujjwal's demand generation: a large part of Project Ujjwal's demand generation was the Ujjwal Saathis (the micro-franchisees), whose impact is not captured by this survey variable. These results, then, may underestimate the likelihood that a woman learned about family planning resources via Project Ujjwal.
Further study should be conducted using a triple difference-in-difference model to estimate whether Project Ujjwal had any effect on closing the disparity in reproductive health access among women of high and low socioeconomic status in Odisha and Bihar. This would provide insight into whether Ujjwal was more effective at targeting high-risk populations than other programs such as Janani Suraksha Yojana, the federal conditional cash transfer for hospital births.8
To more definitively gauge Project Ujjwal's efficacy, further investigation is warranted. Additional analyses would need to assess improvements in health outcomes Project Ujjwal may have generated. Because of gaps in the data, only variables related to reproductive and maternal healthcare uptake were studied. It could be possible that Project Ujjwal positively impacted healthcare uptake but that the care provided did not improve health outcomes. Furthermore, data would need to be obtained on the demand generation of Ujjwal Saathis, e.g., how many products each Ujjwal Saathi sold, how many women each Ujjwal Saathi assisted, etc. To begin the assessment of the program's cost-effectiveness, data would need to be obtained on Ujjwal Saathi's salaries, Project Ujjwal clinic overhead expenses, etc.
6. Conclusion and Implications for Translation
The goal of this work was to summarize key aspects of Project Ujjwal's model and gain a sense of whether public-private partnerships and combined supply- and demand-side interventions could be considered viable models for programs aimed at improving reproductive health in low- and middle-income countries. Results of this work can inform future policy interventions; the preliminary findings presented here suggest that the Project Ujjwal model was effective in augmenting reproductive and maternal healthcare uptake. This study also demonstrates that the program structure pioneered by Project Ujjwal merits further study to determine whether such programs improve health outcomes and to ascertain which aspects of the program most strongly drive healthcare uptake.
While this study has broad ranging implications for women's health initiatives in low- and middle- income countries, it also has important implications for public health interventions specifically within India. The impact of existing federal programs in this space, namely Anganwadi Centers and ASHAs, has been equivocal.20,6 Given the relative dearth of governmental evidence-based reproductive and maternal health interventions operating in India, the Project Ujjwal model seems to be especially worthy of further investigation and potentially, of further implementation.
Compliance with Ethical Standards
Conflicts of interest:
The author declares no competing interests.
Financial Disclosure:
Nothing to declare.
Ethics Approval:
Not applicable.
Disclaimer:
None.
Acknowledgments:
None.
Funding/Support:
There was no funding for this study.
References
- Poor Economics: Rethinking Poverty and the Ways to End It. Random House India; 2013.
- [Google Scholar]
- Contraception as development? New evidence from family planning in Colombia. EconJ. 2010;120(545):709-736. doi:10.1111/j.1468-0297.2009.02306.x
- [CrossRef] [Google Scholar]
- Social norms and the fertility transition. J Dev Econ. 2006;80(1):1-38. doi: 10.1016/j. jdeveco.2005.01.002
- [CrossRef] [Google Scholar]
- Household Bargaining and excess fertility: an experimental study in Zambia. Am Econ Rev. 2014;104(7):2210-2237. doi:10.1257/aer.104.7.2210
- [CrossRef] [Google Scholar]
- Efficiency of Anganwadi Centres-a study in Thiruvananthapuram District, Kerala. J Acad Ind Res. 2014;3(3)
- [Google Scholar]
- The effect of Indian community health workers: multiple tasks and few results. Stanford Digital Repository. Accessed November 7, 2022. https://economics.stanford.edu/effect-indian-community-health-workers-multiple- tasks-and-few-results
- [Google Scholar]
- India's Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet Lond Engl. 2010;375(9730):2009-2023. doi:10.1016/S0140-6736(10)60744-1
- [CrossRef] [PubMed] [Google Scholar]
- Report of the Committee for Evolving a Composite Development Index of States. Working Papers ID: 6728, e Social Sciences 2015 https://ideas.repec.org/pZess/wpaper/id6728.html
- [Google Scholar]
- Ujwal Project: A Multi and Trans-Media Approach to Generating Demand for FP and RH. Johns Hopkins Center for Communication Programs.
- [Google Scholar]
- Status of women in India: a comparison by state. Asia-Pac Popul J. 1993;8(4):59-77.
- [CrossRef] [Google Scholar]
- Community based reproductive health interventions for young married couples in resource- constrained settings: a systematic review. BMC Public Health. 2015;15(1) doi:10.1186/s12889-015-2352-7
- [CrossRef] [PubMed] [Google Scholar]
- International Institute for Population Sciences. Accessed November 8, 2022. http://rchiips.org/nfhs/about.shtml
- [Google Scholar]
- Available Datasets. DHS Program Accessed November 8, 2022. https://dhsprogram.com/data/available-datasets.cfm
- [Google Scholar]
- Census Tables. Office of the Registrar General & Census Commissioner, India. Accessed November 8, 2022. https://censusindia.gov.in/census.website/data/census-tables
- [Google Scholar]
- Exposure to family planning messages and modern contraceptive use among men in urban Kenya, Nigeria, and Senegal: a cross-sectional study. Reprod Health. 2015;12(1) doi:10.1186/s12978-015-0056-1
- [CrossRef] [PubMed] [Google Scholar]
- On kinship structure, female autonomy, and demographic behavior in India. Popul Dev Rev. 1983;9(1):35-60. doi:10.2307/1972894
- [CrossRef] [Google Scholar]
- Quality of maternal healthcare in India: Has the National Rural Health Mission made a difference? J Glob Health. 2011;1(1):79-86.
- [Google Scholar]





