Translate this page into:
Sexually Transmitted Infections in Pre-Exposure Prophylaxis Patients
Abstract
Background and Objective:
Pre-exposure prophylaxis (PrEP) effectively prevents the spread of the human immunodeficiency virus (HIV). HIV is a disease primarily contracted by men who have sex with men or the sharing of needles, syringes, and other drug injection equipment. However, there are some disparities over the thought that PrEP patients have a disproportionate incidence of sexually transmitted infections (STIs) compared with non-PrEP patients. This study aims to clarify the disparity and identify if PrEP patients have a higher incidence of STIs.
Methods:
A survey of 143 respondents was conducted on STI incidence, risk factors, and abstinence from May 13, 2022, to June 20, 2022. The results were analyzed in Statistical Package for the Social Sciences (SPSS V28.0.0.0). SPSS was used to analyze the descriptive statistics associated with STI data obtained from the Naval Medical Readiness and Training Command, Camp Lejeune, Community Health Clinic Patient and Laboratory Tracker.
Results:
This study found a higher incidence of STIs among PrEP patients than non-PrEP patients and a statistical significance (p = 0.010) between the number of partners a person had sex with over the past year and the lifetime incidence of STIs. Portions of the data in the linear regression were used to calculate the significance and can be used as a predictor of STIs based on the number of partners a person has. This can help patients within this community understand their actual risk of contracting an STI based on a potential risk factor.
Conclusion and Implications for Translation:
This study found a higher incidence of STIs among PrEP patients than non-PrEP patients. Additionally, the study can help public health professionals understand the risks associated with military patients who take PrEP and target specific risk factors that influence the disparity in the incidence of STIs. Future studies may use survey data from this study to understand the implications of other risk factors and their association with STIs. Public health professionals can also use these data to develop a predictive index for many risk factors. A predictive index on STI risk is an extremely valuable tool as it allows users to view their risk of obtaining an STI.
Keywords
HIV
Men who have Sex with Men (MSM)
Pre-exposure Prophylaxis (PrEP)
STI
1. Introduction
Previous studies have raised concerns about men who have sex with men (MSM) believing that they do not need prophylaxis during sexual intercourse. This belief increases their risk of acquiring sexually transmitted infections (STIs).1,2,3,4 Previous qualitative studies demonstrated that 35%-60% of pre-exposure prophylaxis (PrEP) users were less likely to use a condom if they were on medication to prevent human immunodeficiency virus (HIV).2,3,4 PrEP does not protect against STIs besides HIV, making this school of thought particularly dangerous. A systematic review and meta-analysis found that most PrEP users are part of a culture or society that promotes an increased risk of obtaining an STI.5 On the other hand, it is easy to view those who use the drug as cautious, taking necessary preventative measures to prevent one disease; thus, they would be the same with other diseases. Some studies show increased STIs among this population, and others are not.6,7 A 2019 study on the Public Health - Seattle & King County STI Clinic found that PrEP users had a higher propensity to contract rectal chlamydia and rectal gonorrhea at 38 per 100 person-years and 20.7 per 100 person-years, respectively. These numbers were statistically significant compared with non-PrEP patients at 10.4 per 100 person-years and 9.8 per 100 person-years, respectively. This study also indicated that the incidence of urethral gonorrhea, syphilis, and pharyngeal chlamydia was higher among PrEP users, although they were not statistically significant.8 Another 2019 study in Chicago on MSM found no statistically significant relationship between PrEP use and an increased risk of contracting an STI through longitudinal, lagged, or mediation models. This study found that PrEP users had a higher propensity to have condom-less sex, but that variable did not increase the mediating model's association between PrEP users and STIs.9
The study among the active duty military population experiences approximately 350 HIV infections annually, with 87% occurring among men who have sex with men. A 2018 survey found that 49% of the military's primary care physicians had poor knowledge of PrEP and only 29% had ever been prescribed the drug. Often, HIV is immediately referred to an infectious disease provider. This helps explain the lack of knowledge among primary care physicians and why, between 2014 and 2016, 60% of U.S. Military Service members prescribed PrEP were administered by an infectious disease provider. This survey also found that 99% of PrEP patients were male, 42% were under 28 years old, 47% were White, 87% were men who had sex with men, 73% did not use a condom, and 30% knowingly had sex with an HIV-positive patient.10 These metrics are startling because the U.S. Military has approximately 1.3 million personnel. Eighty-five percent of these service members are men, of which an estimated 4.23% are men who have sex with men.10 If these numbers tell you one thing, primary care physicians need to understand PrEP and how to use it because high incidences of condomless intercourse among HIV-positive patients drive a need for routine STI testing and ultimately result in an increased incidence of STIs.
To fully understand the ramifications of this study, it is important to consider the culture and values of PrEP patients. One study found that 78% of men who have sex with men met behavioral criteria for HIV prevention medication, but that patient did not accept their risk as being high and rejected the medication.11 Another study on sexual risk found that those who perceived their risk as low had the least knowledge of HIV. People in this community place a stigma on PrEP users rejecting them as potential partners and labeling them with a stereotype of promiscuity. The current culture can contribute to a low incidence of PrEP use in a community with a high risk of getting HIV.12 This is why studies must be clear about the risk factors contributing to STI incidence. It would be a disservice to any researcher, public health professional, or physician to spread discouraging information about a drug that can be 99% effective against HIV if taken in seven doses per week.13
This study aims to determine whether STI incidence is higher among PrEP users than non-PrEP users over 14 months in the Naval Medical Readiness and Training Command (NMRTC), Camp Lejeune, Community Health Clinic. Additionally, this study aims to understand the incidence of STIs, population risk factors, and length of sexual abstinence post-STI using a self-reported patient survey. This study seeks to answer two main research questions: (a) Do PrEP and non-PrEP users have comparable STI incidence? and (b) Can the number of sexual partners a person has been a predictor of STI incidence?
2. Methods
Statistical Package for the Social Sciences (SPSS)14 was used to answer these research questions to analyze the descriptive statistics associated with qualitative STI data obtained from the clinic patient and laboratory tracker. Retrospective data were obtained from January 2021 to March 2022, containing the STI results for 2,532 patients. Access to the data was provided by the Director of Community Health through an internal Excel tracker, which included results for syphilis, urethral gonorrhea, rectal gonorrhea, oral gonorrhea, rectal chlamydia, oral chlamydia, and urethral chlamydia. During the data cleaning process, filters were used to sort results as symptomatic, non-symptomatic, PrEP patients, or non-PrEP patients. Additionally, any data that did not contain responses to all of these variables were excluded from the study.
An in-person paper convenience sampling survey was handed out at patient intake, which produced 143 respondents (93% response rate) from May 13, 2022, to June 20, 2022, on STI incidence, risk factors, and abstinence, and the results were analyzed in SPSS using descriptive statistics and linear regression. The survey consisted of the following questions:
In the past year, have you had sex with? Men, Women, Men, and Women, I have not had sex.
In the past year, how many different partners have you had sex with?______ .
Have you ever had one of the following sexually transmitted infections (STIs): gonorrhea, chlamydia, syphilis, herpes simplex virus, or none of the above?
How many STIs have you had in your lifetime? (no. of STIs). I have never had an STI.
If you have ever had an STI, how long did you abstain from sex?______ (no. of days).
If you have ever had an STI, how long did your partner abstain from sex?_____ (no. of days).
Do you take Truvada for pre-exposure prophylaxis? Yes/No
These two methods were the best way to answer the research question because they target qualitative and quantitative STI incidence, risk factors, and behaviors among PrEP and non-PrEP patients. Institutional Review Board approval (Application Number: 2022-065) was sought from American Public University System, and further approval was provided by the director of NMRTC, Camp Lejeune, Community Health Clinic. This location was selected as it is a central hub for active duty PrEP patients on Camp Lejeune. The survey was not selective in its inclusion and was offered to any patient who sought treatment at the clinic, regardless of age, sex, race, or education.
3. Results
We investigated STI incidence among PrEP and non-PrEP users by combining urethral, rectal, and pharyngeal chlamydia and gonorrhea cases into their respective categories. Figure 1 shows the first research question, “Do PrEP and non-PrEP users have comparable STI incidence?” Overall, there were 115 positive STI cases out of the 304 PrEP patients for a 37.8% (378.3 per 1,000) STI incidence and 546 positive STI cases out of the 2,228 non-PrEP patients for 24.5% (245.06 per 1000) STI incidence. Thus, the incidence of STIs among PrEP patients is 13.3% higher than among non-PrEP patients (Figure 1).
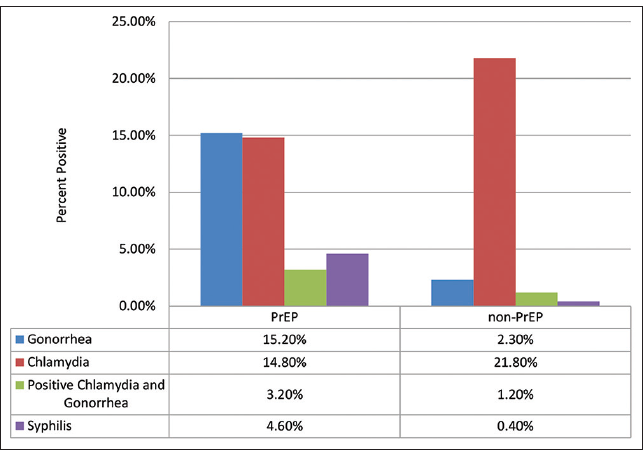
- STI Incidence by PrEP and non-PrEP Use
The only STI that had a higher incidence in non-PrEP patients was chlamydia. This disparity was 5% higher in non-PrEP patients despite PrEP patients being tested for rectal and pharyngeal chlamydia. When comparing only urethral chlamydia among both groups, non-PrEP patients had a 16.1% higher incidence of urethral chlamydia. Another notable variance between both groups was observed in gonorrhea, where PrEP patients had a 14.9% higher incidence. When removing rectal and pharyngeal gonorrhea, because non-PrEP patients were not tested for these STIs and only compared urethral gonorrhea between both groups, non-PrEP patients had a 0.9% higher incidence of urethral gonorrhea (Figure 1).
To answer the second research question, “Can the number of sexual partners a person have been a predictor of STI incidence?” The clinic survey yielded descriptive statistics on the average number of STI respondents had in their lifetime and the average number of partner respondents had in the previous year. Significantly fewer patients reported having an STI, with the majority (51.7%) reporting never having an STI. In this study, 37.8% of respondents reported having at least one STI in their lifetime, leaving only 10.5% of respondents with multiple repeat STIs after initial treatment (Table 1).
| Number of STIsa | Number of respondents | Percent of respondentsb |
|---|---|---|
| 0 | 74 | 51.7 |
| 1 | 54 | 37.8 |
| 2 | 9 | 6.3 |
| 3 | 6 | 4.2 |
Percentages based on 143 respondents.
aNumber of STIs represents the number of previous STIs when reporting to the clinic and completing the survey. This statistic does not include positive results during that visit.
bUnit of measure is the number and percent of people responding to the respective STIs.
Respondents had a narrow range of sexual partners, with 79.7% of respondents having between zero and five sexual partners in the past year. Most of these fell between two and three partners at 18.9% and 19.6%, respectively. The range of partners was between 0 and 30, with the highest number of partners reported by multiple respondents being 10 (4.9%; Table 2). Finding a correlation between the number of sexual partners and the incidence of STIs could prove valuable in educating prospective STI patients at the community health clinic.
| Number of reported partnersa | Number of respondents | Percent of respondentsb | Cumulative percent |
|---|---|---|---|
| 0 | 3 | 2.1 | 2.1 |
| 1 | 24 | 16.8 | 18.9 |
| 2 | 27 | 18.9 | 37.8 |
| 3 | 28 | 19.6 | 57.3 |
| 4 | 18 | 12.6 | 69.9 |
| 5 | 14 | 9.8 | 79.7 |
| 6 | 3 | 2.1 | 81.8 |
| 7 | 5 | 3.5 | 85.3 |
| 8 | 6 | 4.2 | 89.5 |
| 9 | 2 | 1.4 | 90.9 |
| 10 | 7 | 4.9 | 95.8 |
| 11 | 1 | 0.7 | 96.5 |
| 14 | 1 | 0.7 | 97.2 |
| 15 | 1 | 0.7 | 97.9 |
| 17 | 1 | 0.7 | 98.6 |
| 20 | 1 | 0.7 | 99.3 |
| 30 | 1 | 0.7 | 100 |
Percentages based on 143 respondents.
aNumber of partners represents the number of previous partners when reporting to the clinic and completing the survey.
bUnit of measure is the number and percent of people who responded to the respective number of partners.
Linear regression was used to find if a correlation exists between the data in Table 1 (dependent variable) and the data in Table 2 (independent variable). The variable is statistically significant, with a p value of 0.010 (Table 3). We can reject the null hypothesis.15 Table 3 presents an “unstandardized b” of 0.042 for the independent variable, suggesting that each additional sexual partner in this population increases the risk of contracting an STI by 0.042. The coefficient standard error is 0.016, indicating a low spread rate around the regression line.16 Additionally, the “standardized coefficient β” of 0.214 suggests a weak relationship between the dependent and independent variables.17 This indicates no significant correlation between the two variables; however, as previously mentioned, the p value indicates a relationship.
| Question | Unstandardized b | Coefficientsa standard error | Standardized coefficients β | t | p value |
|---|---|---|---|---|---|
| (Constant) | 0.452 | 0.094 | 4.822 | <.001* | |
| In the past year, how many different partners have you had sex with? | 0.042 | 0.016 | 0.214 | 2.596 | 0.010 |
aDependent variable: How many STIs have you had in your lifetime? *p < 0.001 (statistically significant).
4. Discussion
The data analysis and survey were successful in answering both research questions. The first research question explored whether STI incidence levels were comparable between PrEP and nonPrEP users, revealing a significant difference between the two populations. PrEP patients had a marginally higher incidence of STI at 37.8% compared with non-PrEP patients at 24.5%. At the same time, the second question looking at the number of sexual partners a person has had was shown to predict STI incidence. Linear regression analysis between the two variables demonstrated that each new person in this population has sex, with increases their risk of contracting an STI by 0.042. Establishing a predictive value to determine STI risk has a profound impact on the future of community health. A previous study developed disease-specific predictive indexes like the nomogram model for syphilis control practice. This model has been successful in targeting high-risk populations, increasing their syphilis testing, and reducing overall transmission.18
The misinterpretation of PrEP causing increased STI risk is a crucial concern in public health. It is essential to dispel the notion that PrEP increases the likelihood of contracting an STI, considering that MSM accounted for 70% of HIV diagnoses in 2015.19 Discouraging these patients from using PrEP could exacerbate the HIV rate, which is a significant public health issue. The increased STI incidence among PrEP users is likely driven by increased risky sexual behavior within this population.
A study on MSM found that higher rates of condomless anal sex occurred in relationships where one of the partners was on PrEP compared with MSM relationships where no one was on PrEP20 This phenomenon appears to occur because patients perceive the risk of contracting HIV as low when using PrEP and disregard using condoms during sexual intercourse. However, why these patients are not as concerned about contracting bacterial STIs remains unclear. One possible explanation is that these infections are not lifelong and can be easily treated if detected early. Unfortunately, adopting this thought process would inadvertently contribute to the transmission of these diseases. Given the heightened risk faced by this population, the Centers for Disease Control and Prevention (CDC) recommends screening PrEP patients for bacterial STIs every 6 months. A joint modeling study conducted by the CDC and the Rollins School of Public Health indicates that conducting biannual testing for at least 40% of PrEP patients would significantly decrease chlamydia and gonorrhea infections. The same study also revealed that a reduction in condom use by 40% within this population would still result in a 40% reduction in chlamydia cases and a 42% reduction in gonorrhea cases.21 These findings underscore the importance of regular screening and testing to mitigate the spread of STIs among PrEP users.
The observed 13.3% higher incidence of STIs among PrEP patients in this study, combined with the data from the CDC study, may encourage PrEP users to seek regular STL testing. STL testing results in lower transmission of STLs because the patient will stop having intercourse until they are free of the disease. The survey conducted in this study found that 38.5% of respondents abstained from sexual intercourse for at least 14 days, as recommended by the CDC.21 The challenge is getting this information to the public through social media, advertising, or provider handouts.
A predictive index on STI risk is an extremely valuable tool because it allows users to view their risk of obtaining an STI. As seen in this study's linear regression of lifetime STIs versus yearly sexual partners, there is only a small risk 0.042, but when these studies are conducted on other risk factors, such as unprotected sex, that number will change, allowing a user to understand where their highest risk is. Larger and more diverse studies are required to develop a comprehensive predictive index. For example, the data found in this study are particular to the community health clinic population on Camp Lejeune. Different areas around the United States have higher or lower risks of obtaining disease than Camp Lejeune, North Carolina.22 Building a predictive index would take much work, but the struggle would be getting the public to use it. The average user will not seek a peer-reviewed journal to understand their risk of getting an STI but might click an advertisement on Tick-Tok, YouTube, Facebook, or dating applications that link them to the predictive index.23
Although the results of this study are specific to one geographic location, sexually transmitted risk factors and their effect on STI incidence can be generalized to some extent despite variations in transmission rates worldwide. While rates may differ due to cultural, social, and healthcare factors, identifying the increased risk in STI incidence by factor can help to increase willingness to seek testing and ultimately reduce transmission.
The study has several limitations. The study design relies on self-reported data, which may be subject to recall bias or social desirability bias. Participants may have underreported or overstated adherence to preventive measures, leading to inaccuracies in the data collected. Additionally, confounding factors, such as socio-economic status, education level, and access to healthcare, might independently impact STI rates aside from sexual behavior. Selection bias is another potential limitation in this study because the patients were on active duty, had similar financial standings, and could pass an annual fitness test. These factors limit the study from reflecting the broader population of PrEP users. Despite the limitations of this study, future research should examine risk factors, such as condom use, drug use, and history of STDs, to better understand their correlation to STL incidence.
5. Conclusion and Implications for Translation
Based on the findings of our study, the following three key conclusions can be drawn in relation to STl incidence, risk factors, and PrEP use. First, PrEP users had a marginally higher STl incidence rate of 37.8% than 24.5% among non-PrEP patients. Second, the number of sexual partners a person has annually predicted STl incidence, with each additional partner increasing the risk of contracting an STl by 0.042. Lastly, an increased STl incidence among PrEP users is likely driven by risky sexual behavior rather than using PrEP.
These findings have several implications for public health and clinical practice. Healthcare providers need to be knowledgeable about PrEP and the sexual risk factors among those that use it. Because MSM accounts for a significant proportion of HIV diagnoses, discouraging the use of PrEP could negatively impact HIV rates. Instead, the focus should be addressing risky behaviors and promoting safer sexual practices among PrEP users. Additionally, this study suggests that increased testing for bacterial STls, such as chlamydia and gonorrhea, could significantly reduce their transmission in PrEP populations, which highlights the need for healthcare providers to screen PrEP patients regularly and provide appropriate education and counseling regarding the importance of STI testing.
Our results highlight the importance of addressing the high incidence of STls among PrEP users through a multifaceted approach that includes comprehensive sexual education, regular STl testing, and targeted interventions to promote safer sexual practices. By understanding the risk factors associated with STl incidence and adopting evidence-based strategies, public health initiatives and healthcare providers can work toward reducing STl transmission and promoting the overall sexual health and well-being of MSM and PrEP users.
Compliance with Ethical Standards
Conflicts of interest:
The authors declare that this research was conducted to preclude any commercial or financial relationship that might be construed as a conflict of interest.
Financial Disclosure:
Nothing to declare.
Ethics Approval:
The project was approved by the Institutional Review Board (IRB) of American Military University (AMU), American Public University System (APUS), Project Number 2022-065.
Disclaimer:
None.
Acknowledgments:
None.
Funding/Support:
There was no funding for this study.
References
- United Nations Population Fund. Forum on MSM & HIV, United Nations Development Programme. United States Agency for International Development, World Bank. In: Implementing Comprehensive HIV And STI Programmes with Men Who Have Sex With Men: Practical Guidance For Collaborative Interventions. United Nations Development Programme; 2015.
- [Google Scholar]
- Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: a mixed- methods study. AIDS Patient Care STDS. 2012;26(2):87-94. doi: 10.1089/apc.2011.0283
- [CrossRef] [PubMed] [Google Scholar]
- Preexposure prophylaxis and predicted condom use among high-risk men who have sex with men. J Acquir Immune Defic Syndr. 2010;54(5):548-555. doi: 10.1097/QAl.0b013e3181e19a54
- [CrossRef] [PubMed] [Google Scholar]
- Attitudes towards PrEP and anticipated condom use among concordant HIV-negative and HIV-discordant male couples. AIDS Patient Care STDS. 2015;29(7):408-417. doi: 10.1089/apc.2014.0315
- [CrossRef] [PubMed] [Google Scholar]
- Effects of pre-exposure prophylaxis for the prevention of human immunodeficiency virus infection on sexual risk behavior in men who have sex with men: a systematic review and meta-analysis. Clin Infect Dis. 2008;67(5):676-686. doi: 10.1093/cid/ciy182
- [CrossRef] [PubMed] [Google Scholar]
- Confronting rising STIs in the era of PrEP and treatment as prevention. Curr HIV/AIDS Rep. 2019;16(3):244-256. doi: 10.1007/sll904-019-00446-5
- [CrossRef] [PubMed] [Google Scholar]
- Does HIV pre-exposure prophylaxis use lead to a higher incidence of sexually transmitted infections? A case-crossover study of men who have sex with men in Los Angeles, California. Sex Transm Infect. 2018;94(6):457-462. doi: 10.1136/ sextrans-2017-053377
- [CrossRef] [PubMed] [Google Scholar]
- Differences in sexually transmitted infection risk comparing preexposure prophylaxis users and propensity score matched historical controls in a clinic setting. AIDS. 2019;33(11):1773-1780. doi: 10.1097/QAD.0000000000002281
- [CrossRef] [PubMed] [Google Scholar]
- PrEP use and sexually transmitted infections are not associated longitudinally in a cohort study of young men who have sex with men and transgender women in Chicago. AIDS Behav. 2020;24(5):1334-1341. doi: 10.1007/ s10461-019-02664-9
- [CrossRef] [PubMed] [Google Scholar]
- HIV preexposure prophylaxis in the U.S. military services- 2014-2016. MMWR Morb Mortal Wkly Rep. 2018;67(20):569-574. doi: 10.15585/mmwr.mm6720al
- [CrossRef] [PubMed] [Google Scholar]
- Perceptions of pre-exposure prophylaxis (PrEP) among HIV-negative and HIV-positive men who have sex with men (MSM) Cogent Medicine. ;2016Cogent Medicine. ;3:1. doi: 10.1080/2331205X.2016.1256850
- [CrossRef] [Google Scholar]
- Stigma and shame experiences by MSM who take PrEP for HIV prevention: a qualitative study. Am J Mens Health. 2018;12(6):1843-1854. doi: 10.1177/1557988318797437
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of on demand PrEP with TDF-FTC in the ANRS IPERGAY Open-Label Extension Study. 21st International AIDS Conference. 2016.
- [Google Scholar]
- Statistical Package for the Social Sciences. Armonk, NY: IBM Corp. 2022 https://www.ibm.com/products/spssstatistics?utm_content=SRCWW&p1=Search&p4=43700050715561164&p5=e&gdid=Cj0KCQjwk5ibBhDqARIsACzmgLQPQ0mz8tR9u45KWr8ZM1jtOu5Es3GGsFCXY-c2jSLlO-ca_8KDqAaAotNEALw_wcB&gclsrc=aw.ds
- [Google Scholar]
- What the P values really tell us. Korean J Pain. 2017;30(4):241-242. doi: 10.3344/kjp.2017.30.4.241
- [CrossRef] [PubMed] [Google Scholar]
- Regression table. Complete Dissertation by Statistics Solutions. Accessed date? 2022. https://www.statisticssolutions.com/regression-table
- [Google Scholar]
- Standardized Beta Coefficient: Definition & Example. StatisticsHowTo.com: Elementary Statistics for the rest of us! Accessed date? 2022. https://www.statisticshowto.com/ standardized-beta-coefficient
- [Google Scholar]
- Simple-to-use nomogram for predicting the risk of syphilis among MSM in Guangdong Province: results from a serial cross-sectional study. BMC Infect Dis. 2021;21(1) doi: 10.1186/s12879-021-06912-z
- [CrossRef] [PubMed] [Google Scholar]
- HIV Surveillance Report. 2015 Accessed January 30, 2017. Published November 2016. http://www.cdc.gov/hiv/library/reports/surveillance
- [Google Scholar]
- Pre-Exposure Prophylaxis (PrEP) use and condomless anal sex: evidence of risk compensation in a cohort of young men who have sex with men. J Acquir Immune Defic Syndr. 2018;77(4):358-364. doi: 10.1097/ QAI.0000000000001604
- [CrossRef] [PubMed] [Google Scholar]
- CROI 2017 PrEP Study. CDC Accessed date? Released February I5, 2017. https://www.cdc.gov/nchhstp/newsroom/20l7/croi-prepstudy.html#:~:text=More%20than%2040%20percent%20of,condom%20use%20while%20on%20PrEP
- [Google Scholar]
- Animated United States Map Showing Reported Rates of Gonrrhea by State from 2011 to 2020. Sexually transmitted Disease Surveillance. CDC 2020 Accessed date? https://www.cdc.gov/std/statistics/2020/figures/GC-I.htm
- [Google Scholar]
- Social media and health care professionals: benefits, risks, and best practices. PT. 2014;39(7):491-520.
- [Google Scholar]





