Translate this page into:
Examining Trends in Black-White Disparity in Traumatic Spinal Cord Injuries among Pregnancy-Related Hospitalizations in the United States
✉Corresponding author email: deepa.dongarwar@bcm.edu
Abstract
The proportion of women with traumatic Spinal Cord Injuries (tSCI) is increasing globally, yet there is a dearth of data in the literature on female-specific health conditions, such as pregnancy, in this population. In this retrospective cohort study, we sought to fill the gap in the literature regarding racial differences in the trends of tSCI among hospitalized pregnant women. Using Nationwide Inpatient Sample data, all hospitalizations among pregnant women with tSCI were identified. Join point regression analyses were utilized to examine the temporal trends in the rates of tSCI among the entire pregnant hospitalized population in the US during the 10-year study period of 2009-2018. We compared the tSCI hospitalization trends between non-Hispanic (NH) Blacks and NH-Whites. Overall, there was an increase in the rates of tSCI in the entire pregnant population, during the study period (Average annual percentage change [AAPC]: 7.1,95% CI: 1.2, 13.4). The rates of tSCI were consistently higher in NH-Blacks in comparison to NH-Whites. More public health policies should be directed at preventing acute tSCIs during pregnancy and physicians should understand how to meet the needs of pregnant patients with tSCI, especially those who belong to racial/ethnic minority groups.
Keywords
Traumatic Spinal Cord Injury
Racial/Ethnic Disparity
Pregnancy
Hospitalizations
NIS
Temporal Trends
Introduction
Traumatic Spinal Cord Injuries (tSCI) consist of acute damage to the spinal cord often caused by falls or motor vehicle accidents.1 Despite data suggesting that the proportion of women with tSCIs is increasing, there is a dearth of data in the literature on female-specific health conditions, such as pregnancy, in this population.2
Pregnant women with tSCIs experience higher rates of adverse health outcomes such as autonomic dysreflexia, bowel dysfunction, urinary tract infections, deep vein thrombosis, and decubitus ulcers.3 Many of these health issues are life-threatening if proper clinical considerations are not taken. Racial/ethnic minority populations such as African Americans are less likely to undergo surgical treatment, suggesting disparities in the management of the disease.4 It is also likely that mothers from racial/ethnically marginalized sub-populations may disproportionately bear the burden of tSCI although there is no information on the topic. To fill this gap, we examined racial/ethnic rates of tSCIs among pregnant over the previous decade using the US national hospitalization data, a validated dataset with ample sample size.
Methods
We conducted this cross-sectional study using Nationwide Inpatient Sample (NIS) dataset for the years 2009-2018, we conducted this cross-sectional study. The latest available data at the time of the study was for the year 2018. NIS is the largest all-payer hospitalization database in the US, designed to produce national estimates of inpatient utilization, access, cost, quality, and outcomes.5 Each year, the dataset captures information on hospitalizations occurring in 47 states in the US and when weighted, estimates more than 35 million hospitalizations in the country. We included all pregnancy-related hospitalizations in women aged 15-49 years in this study. NIS dataset utilized International Classification of Diseases, Ninth and Tenth Revision, Clinical Modification (ICD-09- CM and ICD-10-CM) codes to define the diagnoses and procedures associated with each hospitalization. Our outcome variable, tSCI, was identified using ICD- 09-CM and ICD-10-CM diagnosis codes based on the recommendations suggested by Noonan et al.6 Race/ethnicity in this study was categorized into non-Hispanic (NH) White and NH-Black. Join point regression, a novel technique for determining the trend of the outcome (tSCI) over time,7 was utilized for this study. The join point regression model assumes a straight line (zero join points) at the beginning of the model building; and iteratively adds single join points, while verifying the statistical significance of the model. Finally, the best model with the optimal number of join points, that achieves statistical significance (p<0.05) is selected. We created join point regression models for the overall pregnant population and then for each racial/ethnic category. The outputs generated from the models were represented as Average Annual Percentage Change (AAPC) and 95% confidence intervals (CI). We used two-tailed hypothesis testing for all statistical analyses, and the type-1 error rate was set at 5%. We utilized R version 3-54 (University of Auckland, Auckland, New Zealand) and RStudio Version 1∙1∙5001 (Boston, MA) to run all statistical analyses. The study was performed on de-identified publicly available data and therefore, was granted exempt status by the Institutional Review Board at Baylor College of Medicine, Texas, United States.
Results
During the study period of 2009-2018, there were a total of 45,498,605 pregnancy-related hospitalizations, out of which, 1,342 (2.9 per 100,000 hospitalizations) had a diagnosis of tSCI. When stratified by race/ ethnicity, we observed that among NH-Whites, there were 686 hospitalizations with tSCI out of 22,395,264 pregnancy-related hospitalizations (3.1 per 100,000 hospitalizations), and among NH-Blacks, there were 246 hospitalizations among a total 6,720,582 pregnancy-related hospitalizations, corresponding to a rate of 3.7 per 100,000 hospitalizations.
Figure 1 shows the rates of tSCI per 100,000 pregnancy-related hospitalizations in the US during the study period of 2009-2018 by race/ethnicity. Overall, there was an increase in the rates of tSCI in the entire pregnant population during the study period (AAPC: 7.1,95% CI: 1.2,13.4). The rates of tSCI were consistently higher in NH-Blacks throughout the study period (13.6 per 100,000 hospitalizations in 2009 to 27.0 per 100,000 hospitalizations in 2018), corresponding to an average annual increase of 7.9% (95% CI: -5.7, 23.5). Among NH-Whites, the tSCI rates were 9.2 per 100,000 hospitalizations in 2009 and increased to 19.4 per 100,000 hospitalizations by 2018, which corresponded to an 8.7% average annual increase (95% CI: 2.4, 15.2).
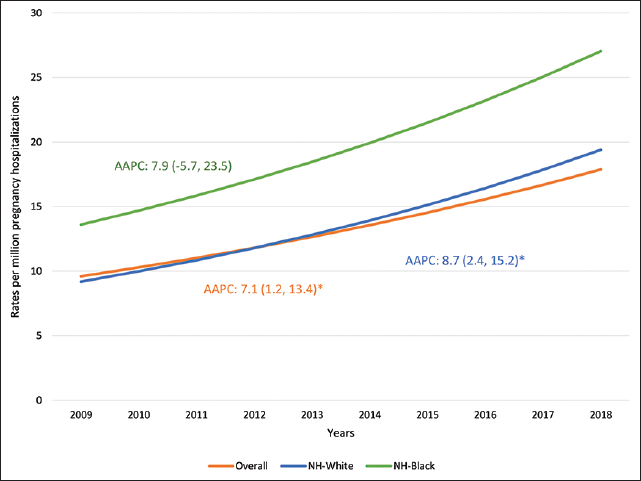
- Trends in rates of tSCI in pregnancy hospitalizations: Black-White Disparity 2009-2018
Discussion, Conclusion, and Implications for Translation
Our study findings suggest that the rates of tSCIs increased across all hospitalized pregnancy populations. This finding is to be expected given the greater awareness of tSCI-associated pregnancy complications and improved knowledge in caring for pregnant women with tSCIs.3 However, the possibility of an increase in acute tSCIs during pregnancy should not be discarded. While previous research has shown that NH-Black patients have higher incidence rates of tSCI than NH-White patients,8 research on tSCIs addressing racial disparities in pregnancy is limited. Our results demonstrate that hospitalization rates related to tSCIs are higher among NH-Black pregnant women compared to NH-White pregnant women. This finding has not been previously reported in the literature and provides insight into this population. Additional research is needed to understand race- specific risk factors for tSCI during pregnancy and to determine if NH-Black pregnant women with tSCIs experience more adverse outcomes than their NH-White counterparts. Furthermore, pregnant patients' ability to access healthcare facilities should be examined to be able to prevent tSCI during pregnancy and to ensure the needs of these vulnerable population is met.
By utilizing the NIS database, this study provides a large sample size of pregnant women with tSCIs and geographical diversity. However, a study limitation is the use of ICD codes since they do not reflect the severity of the tSCI. For those with severe tSCI, there is a greater loss of independence which impacts the quality of life and possibly pregnancy. Given our findings, more public health policies should be directed at preventing acute tSCIs during pregnancy and ensuring physicians understand how to meet the needs of pregnant patients with tSCI. These policies should be inclusive of racial/ethnic minority women and address social determinants of health that are contributing to the racial disparity.
Compliance with Ethical Standards
Conflicts of interest:
None.
Financial Disclosure:
None.
Ethics Approval:
The study was deemed exempt by the Institutional Review Board of Baylor College of Medicine.
Disclaimer:
None.
Acknowledgments:
None.
Funding/Support:
Research funding support was provided by the U.S. Department of Health and Human Services and Health Resources and Services Administration for Baylor College of Medicine Center of Excellence in Health Equity, Training, and Research (Grant No: D34HP3I024).
References
- Traumatic spinal cord injury. Nat Rev Dis Prim. 2017;3(1):1-21.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50(5):365-372.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy outcomes in women with spinal cord lesions. J Obstet Gynaecol Canada. 2013;35(1):39-43.
- [CrossRef] [PubMed] [Google Scholar]
- Race and socioeconomic disparity in treatment and outcome of traumatic cervical spinal cord injury with fracture: Nationwide Inpatient Sample database, 1998-2009. Spinal Cord. 2019;57(10):858-865.
- [CrossRef] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. 2012. Overview of the National (Nationwide) Inpatient Sample (NIS).
- [Google Scholar]
- Linking spinal cord injury data sets to describe the patient journey following injury: a protocol. Top Spinal Cord Inj Rehabil. 2020;26(4):232-242.
- [CrossRef] [PubMed] [Google Scholar]
- Statistical Methodology and Applications Branch, Surveillance Research Program. National Cancer Institute; 2020.
- [Google Scholar]
- Msktc.org. Published 2021 (accessed )





