Translate this page into:
Factors Associated with Utilization of Postnatal Care Services in Mali, West Africa
Abstract
Background and Objective:
Postnatal care is recognized as one of the most effective ways of preventing and managing physical and mental disabilities that occur during the postpartum period. Despite the importance of postnatal care, its utilization is low in Mali. The present study investigates factors associated with utilization of postnatal care services in Mali.
Methods:
A total of 5,778 women who had complete information on all the variables of interest were included in our study. The data were analyzed with Stata version 14.2 by employing a multilevel logistic regression approach. The results were presented using adjusted odds ratios (aOR) at 95% confidence interval (CI).
Results:
We found that 25.18% of childbearing women in Mali utilized postnatal care. Women with no education (aOR=l.28, 95% CI= 1.02-1.62) and those with primary level of education (OR=1.38, 95% CI = 1.06- 1.81) had higher odds of postnatal care uptake, compared to those with secondary/higher education. On the contrary, postnatal care service utilization was lower among women who were not covered by health insurance (aOR=0.63, 95% CI=0.46-0.88), those who were not working (aOR=0.82, 95% CI=0.70-0.96), and those who were not exposed to mass media (aOR=0.80, 95% CI=0.70-0.93). Similarly, compared to women in the Mopti region, women in all other regions were less likely to utilize postnatal care services. Postnatal care service utilization was lower among women in communities with low educational level (aOR = 0.42, 95% CI=0.27-0.66) and medium socio-economic status (aOR=0.59, 95% CI=0.36-0.99).
Conclusion and Implications for Translation:
The study revealed several individual, household and community level factors as predictors of utilization of postnatal care services in Mali. Public health interventions intended to improve postnatal care services uptake in Mali should pay attention to these factors. This will help achieve the Sustainable Development Goal 3.1 which focuses on reducing the global maternal mortality ratio to less than 70 per 100 000 live births by 2030.
Keywords
Women's health
Childbearing women
Mali
Maternal health
Postnatal care services utilization
Public health
Health insurance
Care utilization
Physical health
Mental health
Introduction
Background
The postnatal period is the first six weeks after delivery within which the return of the reproductive organs to their normal non-pregnant state occurs.1 Generally, postnatal care (PNC) is provided to women and their babies within 42 days after delivery.2 The World Health Organization3 recommends that after an uncomplicated vaginal birth in a health facility, healthy mothers and newborns should receive care in the facility for at least 24 hours after birth. On the other hand, if birth is at home, the first postnatal contact should be as early as possible within 24 hours of birth. At least three additional postnatal contacts are recommended for all mothers and newborns, on day 3 (48-72 hours), between 7-14 days after birth, and six weeks after birth.4 PNC is essential to both mothers and their babies. It is widely recognized as one of the most effective ways of preventing and managing physical and mental disabilities that occur during the postpartum period.3,5,6 Thus, lack of PNC service could result in poor health outcomes for both mother and child.7
Despite the importance of PNC, it seems to be neglected in some low- and middle-income countries especially in Africa, where a large number of women do not have access to PNC services.6 For instance, in rural Tanzania, Mohan et al.8 revealed that less than one in four women reported using PNC. Correspondingly, in Uganda, a study that used the 2016 Uganda Demographic and Health Survey revealed that only 50% of women reported having used PNC.9 In Zambia, the prevalence of PNC was reported to be 55%.10 The story is not different in other sub-Saharan African countries such as Ghana,11 Nigeria,12,13 Ethiopia,14 Kenya,7 and Malawi.15 Consequently, a considerable number of women in sub-Saharan Africa (SSA) die of pregnancy-related deaths,16 most of which result from postpartum hemorrhage.17 Besides, SSA records one of the highest neonatal mortality rates globally with 28 deaths per 1,000 live births.18
Previous research has noted the need for further research on increasing access and utilization of postnatal care services, especially in resource-poor settings.19 Some studies conducted in Ghana,20,21 Nigeria,12,22,23 Ethiopia,4,19,24,25 Kenya,7 Tanzania,8,26 Uganda,9 Zambia,10 and Rwanda27 have revealed the determinants of postnatal care services utilization. These studies identified individual (mother's age, educational level, marital status, religion, etc.), household (decision-making capacity for healthcare, wealth quintile and the sex of the head of household) and community-level factors (type of place of residence region, community literacy level, and community socio-economic status) as predictors of postnatal care services utilization.
In Mali, about 31% of maternal deaths occur in the postpartum period.16 Correspondingly, Mali records a high infant mortality rate (54 deaths per 1000 live births), with most of the deaths occurring in the first month of life.28 Despite the high maternal deaths 562 deaths per 100,000 live births in 2017, compared to the global maternal mortality ratio of 211 per 100,000 live births, PNC utilization in Mali is low.29,30
Objectives of the Study
In the present study, we investigate factors associated with utilization of postnatal care services in Mali.
Specific Hypothesis
This study is guided by the hypothesis that individual, household and community level factors are associated with PNC utilization in Mali.
Methods
Study Variables
The study utilized data from the 2018 Mali Demographic and Health Survey. Specifically the data was from the women's file. The DHS is a nationally representative survey that is conducted in over 85 low- and middle-income countries globally. The survey employs a two-stage stratified sampling technique, which makes the data nationally representative. A total of 5,778 women who had complete information on all the variables of interest were included in our study.
The outcome variable for the study was PNC check-up. It was derived from the question, “Did [NAME] go for postnatal checks within 2 months?” The responses were “Yes”, “No”, and “Don't know”. However, only women who provided definite responses (either “Yes” or “No”) were included in the study, where “No”=0 and “Yes”=l. The study used sixteen (16) independent variables. These variables were considered in our study principally because of their statistically significant relationship with PNC utilization in previous studies.10,12,21,22,23 These variables were grouped into individual variables, household variables, and community-level variables. The individual variables included mother's age, educational level, educational level of the mother's partner, marital status, religion, parity, health insurance subscription, employment status, and exposure to mass media. The household variables included decision-making capacity for healthcare, wealth quintile, and the sex of the head of household, while the community-level variables included place of residence, region, community literacy level, and community socio-economic status.
Statistical Analysis
The data were analyzed with Stata version 14.2. The analysis was done in three steps. The first step was the computation of the prevalence of postnatal care in Mali. The second step was a bivariate analysis that calculated the prevalence and proportions of postnatal care across the independent variables with their significance levels. Statistical significance was set at a p-value less than 0.20. To check for a high correlation among the explanatory variables, a test for multicollinearity was carried out using the variance inflation factor (VIF) and the results showed no evidence of high collinearity (Mean VIF= 1.79, Maximum VIF=4.03,and Minimum VIF=1.01). Variables that showed statistical significance in the bivariate analysis were further analyzed using the multilevel logistic regression. In terms of the modelling, four models, comprising the empty model (Model 0), Model 1, Model 2, and Model 3 were fitted hierarchically. Model 0 showed the variance in PNC attributed to the clusters without the explanatory variables. Model 1 contained the individual level factors only, while the household level factors were added to the individual level factors in Model 2. Finally, Model 3 was the complete model that had the individual, household, and community level factors. Adjusted odds ratio (aOR) and associated 95% confidence intervals (CIs) were presented for all the models apart from model 0. We applied sample weight (v005/1,000,000) to correct for over- and under-sampling, and we used the SVY command to account for the complex survey design and generalizability of the findings.
Ethical Approval
This was a secondary analysis of data which did not require further approval since the data is freely available in the public domain. However, the source of data (DHS) reports that ethical clearance was obtained from the Ethics Committee of ORC Macro Inc. as well as Ethics Boards and Ministry of Health of Mali. The DHS is guided by the standards for ensuring the protection of respondents' privacy. Inner City Fund (ICF) International ensured that the survey complies with the U.S. Department of Health and Human Services regulations for the respect of human subjects.
Results
Socio-demographic Characteristics
The results indicate that postnatal care services utilization was high among women aged 40-44 (28.3%), those with secondary/higher education (28.4%) and whose partners had secondary/higher education (33%), cohabiting women (31.2%), Muslims (25.6%), those with one birth (27.2%), those who were covered by National Health Insurance Scheme (48.9%), those who were working (26.5%), and those who were exposed to mass media (26.5%). Furthermore, postnatal care services utilization was high among women in female-headed households (26.4%), those in the richest wealth quintile (34.6%), those who lived in urban areas (33%), those in the Mopti region (50.8%), those in communities with high educational level (33.7%), and those who lived in communities with high socio-economic status (34.1%). At a p-value of 0.20, all the background characteristics of women (except age, marital status, and sex of household head) were significant (Table 1).
| Variables | Frequency | Percentage | PNC (%) | χ2 (p-value) |
|---|---|---|---|---|
| Age | 3.1 (0.798) | |||
| 15-19 | 483 | 8.4 | 24.5 | |
| 20-24 | 1200 | 20.8 | 23.7 | |
| 25-29 | 1500 | 26.0 | 25.0 | |
| 30-34 | 1179 | 20.4 | 25.7 | |
| 35-39 | 891 | 15.4 | 26.3 | |
| 40-44 | 404 | 7.0 | 28.3 | |
| 45-49 | 120 | 2.1 | 22.8 | |
| Education | 16.2 (<0.001) | |||
| No education | 4231 | 73.2 | 24.2 | |
| Primary | 676 | 11.7 | 27.6 | |
| Secondary + | 871 | 15.1 | 28.4 | |
| Partner's education | 45.0 (<0.001) | |||
| No education | 4270 | 73.9 | 23.4 | |
| Primary | 558 | 9.7 | 25.3 | |
| Secondary + | 950 | 16.4 | 33.0 | |
| Marital status | 0.07 (0.790) | |||
| Married | 5745 | 99.4 | 25.2 | |
| Cohabiting | 33 | 0.8 | 31.2 | |
| Religion | 2.4 (0.121) | |||
| Islam | 5395 | 93.4 | 25.6 | |
| Christianity | 383 | 6.6 | 20.0 | |
| Parity | 5.9 (0.116) | |||
| One birth | 866 | 15.0 | 27.2 | |
| Two births | 925 | 16.0 | 24.5 | |
| Three births | 848 | 14.7 | 25.8 | |
| Four or more births | 3138 | 54.3 | 24.7 | |
| Covered by NHIS | 56.2 (<0.001) | |||
| No | 5509 | 95.4 | 24.0 | |
| Yes | 269 | 4.6 | 48.9 | |
| Employment | 5.4 (0.021) | |||
| Not working | 2264 | 39.2 | 22.5 | |
| Working | 3514 | 60.8 | 26.9 | |
| Exposure to mass media | 2.0 (0.153) | |||
| No | 3625 | 62.7 | 24.4 | |
| Yes | 2153 | 37.3 | 26.5 | |
| Decision-making capacity | 17.8 (<0.001) | |||
| Alone | 412 | 7.1 | 38.8 | |
| Not alone | 5366 | 92.9 | 24.1 | |
| Sex of household head | 0.43 (0.514) | |||
| Male | 5104 | 88.3 | 25.0 | |
| Female | 674 | 11.7 | 26.4 | |
| Wealth quintile | 110.7 (<0.001) | |||
| Poorest | 1168 | 20.2 | 29.6 | |
| Poorer | 1241 | 21.5 | 21.9 | |
| Middle | 1249 | 21.6 | 18.9 | |
| Richer | 1115 | 19.3 | 22.7 | |
| Richest | 1005 | 17.4 | 34.6 | |
| Place of residence | 91.5 (<0.001) | |||
| Urban | 1145 | 19.8 | 33.0 | |
| Rural | 4633 | 80.2 | 23.3 | |
| Region | 377.1 (<0.001) | |||
| Kayes | 921 | 15.9 | 23.1 | |
| Koulikoro | 1112 | 19.3 | 19.5 | |
| Sikasso | 1067 | 18.5 | 9.3 | |
| Segou | 919 | 15.9 | 26.9 | |
| Mopti | 622 | 10.8 | 50.8 | |
| Toumbouctou | 221 | 3.8 | 14.4 | |
| Gao | 149 | 2.6 | 33.5 | |
| Kidal | 3 | 0.1 | 37.2 | |
| Bamako | 763 | 13.2 | 36.7 | |
| Community educational level | 72.9 (<0.001) | |||
| Low | 2386 | 41.3 | 21.1 | |
| Medium | 1889 | 32.7 | 23.6 | |
| High | 1503 | 26.0 | 33.7 | |
| Community socio-economic status | 105.0 (<0.001) | |||
| Low | 3782 | 65.5 | 23.4 | |
| Medium | 632 | 10.9 | 16.8 | |
| High | 1364 | 23.6 | 34.1 | |
Source: 2018 Mali Demographic and Health Survey
Prevalence of Postnatal Care Services Utilization Among Childbearing Women in Mali
The results show that a little over a quarter (25.18%) of childbearing women in Mali utilized postnatal care services (Figure 1).
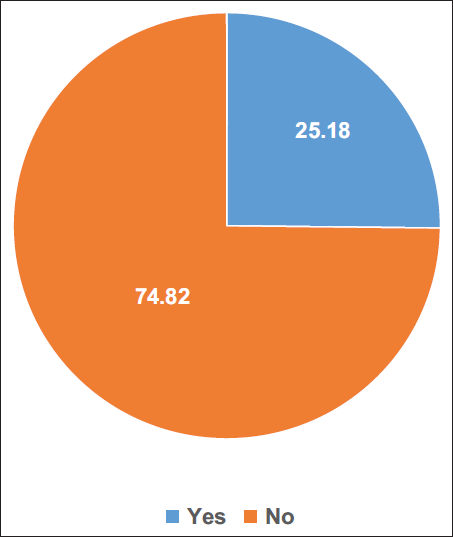
- Prevalence of postnatal care services utilization among childbearing women in Mali
Factors Associated with Postnatal Care Services Utilization Among Childbearing Women in Mali
Women with no formal education (aOR= 1.28, 95% CI= 1.02-1.62) and those with primary level of education (aOR=l.38, 95% CI=1.06-1.81) had higher odds of postnatal care uptake, compared to those with secondary/higher education. On the contrary, postnatal care services utilization was lower among women who were not covered by health insurance (aOR=0.63, 95% CI=0.46-0.88), those who were not working (aOR=0.82, 95% CI=0.70-0.96), and those who were not exposed to mass media (aOR=0.80, 95% CI=0.70- 0.93), compared to those who were covered by health insurance, those who were working, and those who were exposed to mass media, respectively. Similarly, compared to women in the Mopti region, women in all other regions were less likely to utilize postnatal care services. Postnatal care services utilization was also lower among women in communities with low educational level (aOR = 0.42, 95% CI=0.27-0.66) and those in communities with medium socio-economic status (aOR=0.59, 95% CI=0.36-0.99) compared to those in high educational level and socio-economic status communities, respectively (Table 2).
| Variables | Model 0 | Model 1 aOR [95%CI] | Model 2 aOR [95%CI] | Model 3 aOR [95%CI] |
|---|---|---|---|---|
| Education | ||||
| No education | 1.20 (0.95-1.51) | 1.29* (1.03-1.63) | 1.28* (1.02-1.62) | |
| Primary | 1.30 (0.99-1.70) | 1.38* (1.05-1.80) | 1.38* (1.06-1.81) | |
| Secondary + | 1 | 1 | 1 | |
| Partner's education | ||||
| No education | 0.75** (0.60-0.93) | 0.80 (0.64-1.00) | 0.81 (0.68-1.01) | |
| Primary | 0.82 (0.62-1.09) | 0.87 (0.66-1.15) | 0.88 (0.67-1.16) | |
| Secondary + | 1 | 1 | 1 | |
| Religion | ||||
| Islam | 1 | 1 | 1 | |
| Christianity | 0.80 (0.56-1.15) | 0.80 (0.56-1.16) | 0.90 (0.63-1.29) | |
| Parity | ||||
| One birth | 1.06 (0.84-1.34) | 1.05 (0.83-1.34) | 1.07 (0.84-1.35) | |
| Two births | 0.88 (0.69-1.10) | 0.88 (0.69-1.11) | 0.88 (0.70-1.11) | |
| Three births | 1 | 1 | 1 | |
| Four or more births | 0.89 (0.73-1.08) | 0.89 (0.73-1.08) | 0.91 (0.75-1.10) | |
| Covered by NHIS | ||||
| No | 0.58** (0.41-0.81) | 0.63** (0.45-0.88) | 0.63** (0.46-0.88) | |
| Yes | 1 | 1 | 1 | |
| Employment | ||||
| Not working | 0.86 (0.75-1.02) | 0.88 (0.75-1.03) | 0.82* (0.70-0.96) | |
| Working | 1 | 1 | 1 | |
| Exposure to mass media | ||||
| No | 0.81** (0.70-0.94) | 0.82** (0.71-0.94) | 0.80** (0.70-0.93) | |
| Yes | 1 | 1 | 1 | |
| Decision-making capacity | ||||
| Alone | 1 | 1 | ||
| Not alone | 0.84 (0.64-1.10) | 0.87 (0.67-1.14) | ||
| Wealth quintile | ||||
| Poorest | 0.65** (0.47-0.89) | 0.79 (0.52-1.19) | ||
| Poorer | 0.60** (0.44-0.82) | 0.79 (0.53-1.18) | ||
| Middle | 0.52*** (0.39-0.71) | 0.72 (0.49-1.06) | ||
| Richer | 0.66** (0.51-0.84) | 0.78 (0.59-1.03) | ||
| Richest | 1 | 1 | ||
| Place of residence | ||||
| Urban | 1 | |||
| Rural | 1.18 (0.75-1.88) | |||
| Region | ||||
| Kayes | 0.31*** (0.20-0.49) | |||
| Koulikoro | 0.22*** (0.14-0.35) | |||
| Sikasso | 0.10*** (0.06-0.16) | |||
| Segou | 0.39*** (0.25-0.61) | |||
| Mopti | 1 | |||
| Toumbouctou | 0.18*** (0.11-0.31) | |||
| Gao | 0.55* (0.33-0.94) | |||
| Kidal | 1.06 (0.54-2.05) | |||
| Bamako | 0.37*** (0.21-0.64) | |||
| Community educational level | ||||
| Low | 0.42*** (0.27-0.66) | |||
| Medium | 0.57** (0.38-0.85) | |||
| High | 1 | |||
| Community socio-economic status | ||||
| Low | 1.25 (0.75-2.09) | |||
| Medium | 0.59* (0.36-0.99) | |||
| High | 1 | |||
| Random effect results | ||||
| PSU variance (95% CI) | 1.13 (0.89-1.44) | 1.09 (0.86-1.39) | 1.00 (0.78-1.28) | 0.53 (0.39-0.71) |
| ICC | 25.6% | 24.9% | 23.2% | 13.8% |
| LR Test | χ2=479.21, p=0.000 | χ2=436.70, p=0.000 | χ2=374.96, p=0.000 | χ2=162.53, p=0.000 |
| Wald chi-square | 40.9 | 61.8 | 226.1 | |
| Model fitness | ||||
| Log-likelihood | -2982.4 | -2962.0 | -2951.8 | -2881.7 |
| AIC | 5968.7 | 5950.0 | 5939.7 | 5825.3 |
| N | 5778 | 5778 | 5778 | 5778 |
***p<0.001,**p<0.05,*p<0.10
Discussion
In the present study, we investigated the utilization of PNC services which include provision of immunizations such as BCG, OPV and hepatitis B vaccines, promotion of birth spacing, continuous exclusive breastfeeding practices, and early postnatal contact in Mali. The study recorded 25.2% prevalence of PNC service utilization in Mali. This prevalence is lower than what was recorded in Kenya (47%),7 rural Ghana (62%),11 northwest Ethiopia (57.5%),25 and Uganda (50%).9 It is, however, higher than what was reported in northern Ethiopia (8%)19 and rural Tanzania (10.4%).26 The study also reveals an association between postnatal care services uptake and factors such as maternal education, health insurance subscription, employment status, mass media exposure, region of residence, and level of community education and socio-economic status.
Women with no formal education and those with primary level of education had adjusted higher odds of PNC uptake, compared to those with secondary/higher education. Contrary to this finding, most previous studies reveal that utilization of PNC services increases with attainment of higher levels of education. For instance, Akunga et al.7 found that lack of formal education was associated with low use of postnatal care services. Other studies have reported direct association between higher education and increased PNC service utilization.9,10,12,13,14,19,25 Conversely, postnatal care services utilization was also lower among women in communities with low educational level and those in communities with medium socio-economic status, compared to those in high educational level and socio-economic status communities, respectively. Communities with poor education and low socio-economic status, on the contrary, are characterized by health infrastructure deficit, which limits access to healthcare services, such as postnatal care. This finding resonates with findings of some previous studies.7,9,10,12,19
The study also reports lower odds of postnatal care services utilization among women without health insurance, compared with those with health insurance. This finding is consistent with some previous studies which noted a direct relationship between health insurance subscription and higher odds of postnatal care services utilization. In Nigeria, Dahiru and Oche22 reported that health insurance subscription increases the likelihood of the utilization of postnatal care services among women. Similarly, Browne et al.21 revealed that utilization of postnatal care services among women with health insurance in Ghana increased by 61%. Rwabufigiri et al.27 also revealed that health insurance subscription is likely to increase the utilization of postnatal care services in Rwanda. Thus, to ensure an increase in postnatal care services utilization in Mali, it is critical for the Malian government to make attempts to expand the health insurance coverage in the country. More importantly, there should be a waiver of subscription premium for women accessing maternal healthcare services, especially postnatal care.
Additionally, those who were not working recorded lower odds of postnatal care services utilization, compared with those who were employed. This finding is consistent with findings of some previous studies. Berhe et al.,19 for instance, revealed that mothers' employment was significantly associated with utilization of postnatal care services among women in Ethiopia. Similarly, Ndugga et al.9 identified mothers' employment status as a determinant of the utilization of postnatal care services in Uganda. Overall, these studies reveal that being employed increases women's likelihood of using postnatal care services. This suggests that employment gives women some form of financial autonomy that helps them overcome financial barriers that are likely to obstruct utilization of postnatal care services.
The study also revealed that women without mass media exposure were less likely to use postnatal care services, compared with those with mass media exposure. This finding highlights the significant role played by the mass media in health promotion. Studies have revealed that the mass media serve as a channel through which health information reaches people.9,10
This finding suggests the need for health promotion programs to use the mass media as a channel to provide information on postnatal care services utilization to women. Also, there is a need for women to be encouraged to use the mass media, so as to get access to such information. This association between exposure to mass media and uptake of postnatal care services has been reported in other studies.9,10,12,19
Compared to women in the Mopti region, women in all other regions were less likely to utilize postnatal care services. This finding is surprising, given that Mopti is a deprived region in Mali, with most of its residents living in rural areas with the lowest level of education in the country.20 Thus, it is unclear the possible reason for this finding. We, therefore, suggest that further research be conducted to explore reasons for this finding. Such a study could be qualitative so as to allow in-depth explorations of the matter. Some previous studies have also reported an association between region of residence and utilization of postnatal care services.7,13,14,20
Strengths and Limitations of the study
The main strength of the study lies in its use of a nationally representative data. As such, generalizability of the findings to women in the entire nation is guaranteed. Relatedly, the findings could be a reflection of the current state of affairs, since the study used the most recent version of the Mali Demographic and Health Survey. Moreover, the survey relied on best data collection methods, featuring highly experienced field assistants. Despite these strengths, it is prudent for the findings to be seen in the light of certain limitations. First, the study employed a cross-sectional study design, which prevents us from making causal inferences among the studied variables. Additionally, the study suffers from recall biases that characterize demographic and health survey data.
Conclusion and Implications for Translation
The study revealed several individual, household and community level factors as predictors of utilization of postnatal care services in Mali. Public health interventions intended to improve postnatal care services uptake in Mali pay attention to these factors. This will help achieve the Sustainable Development Goal 3.1 which focuses on reducing the global maternal mortality ratio to less than 70 per 100 000 live births by 2030.
Compliance with Ethical Standards
Conflicts of interests:
The authors declare no competing interest.
Financial disclosure:
Nothing to declare.
Ethics approval:
Ethics approval was not required for this study since the data is secondary and is available in the public domain. More details regarding DHS data and ethical standards are available at: http://goo.gl/ny8T6X.
Disclaimer:
The publication of this article was supported by the Global Health and Education Projects, inc. (GHEP) through the Emerging Scholar's Grant Program (ESGP). The information, contents, and conclusions are those of the author(s) and should not be construed as the official position or policy of, nor should any endorsements be inferred by ESGP or GHEP.
Acknowledgments:
The authors thank the MEASURE DHS project for their support and for free access to the original data.
Funding/support:
There was no funding for this study.
References
- Factors associated with postnatal care utilization among postpartum women in Ethiopia: a multi-level analysis of the 2016 Ethiopia demographic and health survey. Arch Public Health. 2020;78:34.
- [CrossRef] [PubMed] [Google Scholar]
- Delivering contraceptive vaginal rings: Review of postpartum and postnatal care programs in Nigeria. Abuja:Population Council 2015
- [CrossRef] [Google Scholar]
- WHO recommendations on newborn health: guidelines approved by the WHO Guidelines Review Committee:World Health Organization. 2017.
- [Google Scholar]
- Determinants of postnatal care service utilization in diga district, east wollega zone, wester Ethiopia: case-control study. Ethiopian Journal of Reproductive Health. 2018;10(4):52-61.
- [Google Scholar]
- Utilization of maternal postnatal care services among women in selected villages of Bahi District in Tanzania. Curr Res J Soc Sci. 2015;7(4):106-111.
- [CrossRef] [Google Scholar]
- Geneva: World Health Organization; 2014.
- Determinants of postnatal care use in Kenya. African Population Studies. 2014;28(3):1447-1459.
- [CrossRef] [Google Scholar]
- Determinants of postnatal care use at health facilities in rural Tanzania: Multilevel analysis of household survey. BMC Pregnancy Childbirth. 2015;15:282.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of early postnatal care attendance: analysis of the 2016 Uganda demographic and health survey. BMC Pregnancy Childbirth. 2020;20(1):163.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with postnatal care for newborns in Zambia: analysis of the 2013- -14 Zambia demographic and health survey. BMC Pregnancy Childbirth. 2017;17(1):418.
- [CrossRef] [PubMed] [Google Scholar]
- The role of community- based health services in influencing postnatal care visits in the Builsa and the West Mamprusi districts in rural Ghana. BMC Pregnancy Childbirth. 2018;18(1):295.
- [CrossRef] [PubMed] [Google Scholar]
- Population attributable risk estimates for factors associated with non-use of postnatal care services among women in Nigeria. BMJ Open. 2016;6(7):e010493.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of postnatal care non-utilization among women in Nigeria. BMC Res Notes. 2016;9(1):21.
- [CrossRef] [PubMed] [Google Scholar]
- Spatial patterns and determinants of postnatal care use in Ethiopia: findings from the 2016 demographic and health survey. BMJ Open. 2019;9(6):e025066.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of postnatal service utilisation among mothers in rural settings of Malawi. Health Soc Care Community. 2015;23(5):493-501.
- [CrossRef] [PubMed] [Google Scholar]
- Timing of maternal death: levels, trends, and ecological correlates using sibling data from 34 sub- Saharan African countries. PLoS One. 2018;13(1):e0189416.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with postpartum hemorrhage maternal death in referral hospitals in Senegal and Mali: a cross- sectional epidemiological survey. BMC Pregnancy Childbirth. 2015;15(1):235.
- [CrossRef] [PubMed] [Google Scholar]
- Provision of postpartum care to women giving birth in health facilities in sub-Saharan Africa: A cross-sectional study using Demographic and Health Survey data from 33 countries. PLoS Med. 2019;16(10):e1002943.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of postnatal care utilization in Tigray, Northern Ethiopia: A community based cross-sectional study. PLoS One. 2019;14(8):e0221161.
- [CrossRef] [PubMed] [Google Scholar]
- The socio-economic determinants of maternal health care utilization in Ghana. Int J Soc Econ. 2011;38(7):628-48.
- [CrossRef] [Google Scholar]
- Health insurance determines antenatal, delivery and postnatal care utilisation: evidence from the Ghana Demographic and Health Surveillance data. BMJ Open. 2016;6(3):e008175.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr Med J. 2015;21:321.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal and community factors associated with unmet contraceptive need among childbearing women in Northern Nigeria. Contracept Reprod Med. 2019;4:11.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with postnatal care utilization among postpartum women in Ethiopia: a multi-level analysis of the 2016 Ethiopia demographic and health survey. Arch Public Health. 2020;78:34.
- [CrossRef] [Google Scholar]
- Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):508.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with compliance with the recommended frequency of postnatal care services in three rural districts of Tanzania. BMC Pregnancy Childbirth. 2015;15(1):341.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with postnatal care utilisation in Rwanda: A secondary analysis of 2010 Demographic and Health Survey data. BMC Pregnancy Childbirth. 2016;16(1):122.
- [CrossRef] [PubMed] [Google Scholar]
- 2018 Mali Demographic and Health Survey Key Findings. Rockville, Maryland, USA: INSTAT and ICF; 2019.
- Determinants of maternal healthcare utilization among married adolescents: Evidence from 13 Sub-Saharan African countries. Public Health. 2019;177:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Correlates of maternal healthcare service utilisation among adolescent women in Mali: analysis of a nationally representative cross-sectional survey, 2006. Journal of Public Health. 2013;21(1):15-27.
- [CrossRef] [Google Scholar]





