Translate this page into:
Barriers and Facilitators to Accessing Health Care Services among Married Women in Ethiopia: a Multi-level Analysis of the Ethiopia Demographic and Health Survey
✉Corresponding author email: sanni.yaya@uottawa.ca
Abstract
Background and Objective:
Access to health care services is a major challenge to women and children in many developing countries such as Ethiopia. In this study, we investigated the individual- and community- level factors associated with barriers to accessing health care services among married women in Ethiopia.
Methods:
Data from the 2016 Ethiopia demographic and health survey on 9,824 married women of reproductive age (15-49 years) were analyzed. Multilevel logistic regression models were used to assess individual- and community-level factors associated with barriers to access health care services. Regression analysis results revealed adjusted odds ratios at 95% confidence intervals.
Results:
Over two-thirds (71.8%) of married women in Ethiopia reported barriers to accessing health care services. Some of the individual-level factors that were associated with lower odds of reporting barriers to access health care services include: having secondary education (aOR=0.49, 95% CI: 0.32-0.77), being in the richest quintile (aOR=0.34, 95% CI: 0.22-0.54), and indicating wife-beating as unjustified (aOR=0.66, 95% CI: 0.55-0.81). Among the community-level factors, high community-level literacy (aOR=0.56, 95% CI: 0.34-0.92) and moderate community socioeconomic status (aOR=0.62, 95% CI: 0.45-0.85) were significantly associated with lower odds of reporting barriers to access health care services.
Conclusion and Implications for Translation:
The findings revealed high barriers to access health care services, and both individual- and community-level factors were significant contributing predictors. Therefore, it is important to consider multidimensional strategies and interventions to facilitate access to health care services in Ethiopia.
Keywords
Health Care Access
Factors
Multilevel
Ethiopia
DHS
Global Health
Individual- and Community-Levels
Barriers
Facilitators
Introduction
Background of the Study
Access to health care services is a fundamental human right, and barriers to accessing health services may have a detrimental effect on an individual's physical and mental health, and overall quality of life.1,2 Delays in receiving quality health care services, unnecessary financial expenditures, preventable hospitalization, and unmet health needs are strongly associated with barriers to access health care services.1 Regrettably, access to health care services is a common problem in developing countries.1,3
Globally, approximately 400 million people do not have access to health care services, and about eight million deaths are treatable health problems.4 Only half of the population in Africa have access to modern health facilities,5 mainly due to financial burdens and geographic distance.6 Zegeye et al. (2021) revealed that geographic distance to a health facility, money, and garnering permission from the husband were reasons for the inaccessibility to health services for women in Benin.7
In Ethiopia, access barriers to health care services are prevalent in rural communities. The implementation of the primary health care (PHC) services through the rapid expansion of health centers and health posts, as well as training and recruiting primary and middle-level health professionals, were some of the attempts made to reduce access barriers.8 The program significantly improved PHC coverage from 76.9% in 2005 to 90% in 2010.8 However, regional disparities and socioeconomic inequalities continue to exist in accessing health services, particularly for those living in rural areas.9 Several factors such as women's empowerment,10 religion,11 place of residence,12,13 region,14 as well as physician preference and service acceptability by patients10,15 are known to play a significant role in health service accessibility.
The few studies on health service accessibility in Ethiopia focus on facility and health force distribution,9 cultural factors and health-seeking behavior,16 physical accessibility,17 and descriptive reports. However, no comprehensive study to date exists on the individual- and community- level factors associated with health care service accessibility barriers in Ethiopia. In this study, multilevel modeling was applied to investigate the effects of cluster-level (i.e., primary sampling units) variables on individual-level outcomes (i.e., reporting barriers to access health care services by respondent). Multilevel modeling was also used to explore the effects of specific community-level characteristics (residence, region, literacy level in the community, and socioeconomic status of the community) on reported barriers to access health care services, while also adjusting for individual-level factors.
Objectives of the Study
We used nationally representative data to examine the individual- and community-level factors associated with barriers to access health care services among married women of reproductive age (15-49) living in Ethiopia. We hypothesize that both individual- and community-level factors are associated with barriers to access health care services among married women of reproductive age (15-49) living in Ethiopia.
Methods
Study Variables
Data from the 2016 Ethiopia demographic and health survey (EDHS) were used to conduct this study. Using a two-stage stratified cluster sampling method, the data included men and women in their reproductive age. First, enumeration areas (EAs) were selected using Probability Proportional to Size (PPS).18 Second, household selection and interviews took place; 16,650 out of 18,008 households were interviewed resulting in the participation of a total of 15,683 women aged 15-49 years.18 Survey methodology details are in the final report.18 The final analysis in this study was limited to married women (N=9824).
The outcome variable for this study was barriers to access health care services. In the survey, women were asked the following question with four options to assess factors that prevent women from getting medical advice or treatment as an indication of access to health care services: “When you are sick and want to get medical advice or treatment, is each of the following a big problem or not? (1) Getting permission to go to the doctor? (2) Getting money needed for advice or treatment? (3) The distance to the health facility? (4) Not wanting to go alone?”18 The outcome variable was coded as “yes” if a woman encountered at least one of the aforementioned problems. Those who did not have any problem were considered not to have barriers in access to health care services and coded as “no.”
Individual- and community-level factors were considered as independent variables. The individual- level factors included age (15-19, 20-24, 25-29, 30-34, 35-39, 40-44, 45-49), women's and husband's educational level (no formal education, primary school, secondary school, higher), women's and husband's occupation (not working, professional or technical or managerial, clerical, sales, agricultural- employee, services, skilled manual, unskilled manual, others), wealth index (poorest, poorer, middle, richer, richest), media exposure (no, yes), religion (Orthodox, Protestant, Muslim, Others), parity (no, 1-2, 3-4, 5+), family size (<5, >=5), sex of household head (male, female), native language (Amarigna, Tigregna, Oromigna, Afarigna, Somaligna, Sidamigna, Agniwakigna, Nuwerigna/Gambeligna, Gumuzigna/Bangagna, Others), decision making (no, yes) and wife-beating (accept, refuse).
Community-level factors included place of residence (urban, rural), region (Tigray, Afar, Amhara, Oromia, Somali, Benishangul, SNPPR, Gambela, Harari, Addis Ababa, Dire Dawa), literacy level (low, medium, high), and socioeconomic status (low, moderate, high). A given community's participants' wealth, education, and occupation were aggregated to create the community socioeconomic status variable. Principal component analysis was used to estimate women who were poor, uneducated, and unemployed, resulting in a standardized score with a mean (0) and standard deviation (1). These were then categorized into tertile 1 (the lowest scores, least disadvantaged, and highest socioeconomic status), tertile 2, and tertile 3 (highest scores, most disadvantaged, and lowest socioeconomic status). Similarly, for community literacy, respondents who had attended higher than secondary school were assumed to be literate while all other respondents were given a sentence to read, and they were considered literate if they could read all or part of the sentence.18 Therefore, high literacy included respondents who had higher than secondary education or had no school/primary/secondary education and could read a whole sentence. Medium literacy were respondents who had no school/primary/secondary education and could read part of the sentence. Low literacy were respondents who had no school/primary/secondary education and could not read at all. These were categorized into appropriate tertiles where tertile 1 (lowest score, least disadvantaged) was high community literacy, tertile two (medium score) was medium community literacy, and tertile 3 (highest score, most disadvantaged) was low community literacy.
Statistical Analysis
Descriptive statistics were performed to obtain the frequency and percentages of all variables and the prevalence of barriers to health care services. Subsequently, bivariate analysis (chi-square test) was completed to select potential variables for the regression analysis. A p-value less than 0.05 was used as a cut-off point. Using the variance inflation factor (VIF), a multi-collinearity test was performed for all explanatory variables that had a significant association with the outcome variable. The test revealed no evidence of collinearity between explanatory variables (Mean VIF =1.82, Min VIF=1.03, Max VIF=3.59). To account for the DHS's complex sampling design for data collection, the appropriate level-weights in DHS surveys were used at the individual level 1 and cluster (community) level 2.
A multilevel logistic regression model (MLRM), which consisted of fixed and random effects was fitted in the final step.19 The fixed effects revealed the association between the independent variables and the outcome variable and were reported as adjusted odds ratios (AOR) with 95% confidence intervals (CIs). Measures of variations, known as random effects, were assessed using Intra-Cluster Correlation (ICC). The Likelihood Ratio (LR) tested model adequacy and Akaike's Information Criterion (AIC) measured how well the different models fitted the data on the four models.
The first model - Model 0 - was the empty model used to check the variance in the outcome variable attributed to the clustering of primary sampling units (PSUs) (Model 0). The second model - Model I - included individual-level factors associated with barriers in accessing health care services. In the third - Model II - community-level factors were fitted. The fourth - Model III - included both the individual- and community-level factors. All analyses were weighted to adjust for the DHS sampling design. The data were analyzed with STATA Version 14.
Ethical Approval
This study used publicly available secondary data from the DHS Program which ensures standards are followed for the protection of respondents' privacy and confidentiality. Details regarding ethical considerations and the protection and privacy of DHS survey respondents are available at: http://goo.gl/ny8T6X.
Results
Sociodemographic Characteristics
Table 1 reveals a total of 9,824 married women were included in this study, of whom, 23.5% were in the 25-29-year-old age group. More than three- quarters (83.8 %) resided in rural areas and 61.2% had no formal education. Over half (51.6 %) of the participants were unemployed, and more than one- fifth (23.5 %) had worked in agriculture. Over three- fifth (61.7 %) were not exposed to any form of media (i.e., newspaper, radio, or television).
| Variables | Number (Weighted %) | Barrier in access to health care | P-value | |
|---|---|---|---|---|
| No, Number (Weighted %) | Yes, Number (Weighted %) | |||
| Age in years | P=0.4707 | |||
| 15-19 | 664 (5.75) | 230 (30.37) | 434 (69.63) | |
| 20-24 | 1,783 (16.72) | 645 (28.92) | 1,138 (71.08) | |
| 25-29 | 2,236 (23.50) | 748 (29.47) | 1,488 (70.53) | |
| 30-34 | 1,854 (20.04) | 607 (27.51) | 1,247 (72.49) | |
| 35-39 | 1,565 (15.78) | 510 (28.38) | 1,055 (71.62) | |
| 40-44 | 1,019 (10.40) | 315 (26.80) | 704 (73.20) | |
| 45-49 | 703 (7.81) | 200 (23.84) | 503 (76.16) | |
| Women's educational level | P<0.001 | |||
| No formal education | 5,693 (61.17) | 1,367 (21.79) | 4,326 (78.21) | |
| Primary school | 2,700 (28.31) | 1,008 (29.76) | 1,692 (70.24) | |
| Secondary school | 880 (6.40) | 510 (59.03) | 370 (40.97) | |
| Higher | 551 (4.12) | 370 (63.50) | 181 (36.50) | |
| Husband educational level | P<0.001 | |||
| No formal education | 4,524 (46.59) | 1,090 (22.52) | 3,434 (77.48) | |
| Primary school | 3,054 (36.90) | 956 (25.67) | 2,098 (74.33) | |
| Secondary school | 1,226 (9.54) | 587 (43.48) | 639 (56.52) | |
| Higher | 1,020 (6.97) | 622 (57.96) | 398 (42.04) | |
| Women occupation | P<0.001 | |||
| Not working | 5,345 (51.60) | 1,606 (23.71) | 3,739 (76.29) | |
| Professional or technical or managerial | 270 (2.30) | 168 (55.37) | 102 (44.63) | |
| Clerical | 88 (0.63) | 69 (80.99) | 19 (19.01) | |
| Sales | 1,320 (13.21) | 606 (38.17) | 714 (61.83) | |
| Agricultural employee | 1,916 (23.45) | 445 (25.78) | 1,471 (74.22) | |
| Services | 219 (2.62) | 96 (22.80) | 123 (77.20) | |
| Skilled manual | 355 (3.76) | 147 (39.55) | 208 (60.45) | |
| Unskilled manual | 130 (0.81) | 40 (32.20) | 90 (67.80) | |
| Others | 181 (1.62) | 78 (43.17) | 103 (56.83) | |
| Husband occupation | P<0.001 | |||
| Not working | 1,158 (9.07) | 271 (22.22) | 887 (77.78) | |
| Professional or technical or managerial | 774 (5.22) | 393 (47.87) | 381 (52.13) | |
| Clerical | 92 (0.62) | 58 (50.13) | 34 (49.87) | |
| Sales | 782 (6.99) | 388 (39.58) | 394 (60.42) | |
| Agricultural employee | 4,891 (61.88) | 1,192 (22.60) | 3,699 (77.40) | |
| Services | 432 (3.10) | 200 (43.67) | 232 (56.33) | |
| Skilled manual | 888 (6.88) | 469 (45.73) | 419 (54.27) | |
| Unskilled manual | 366 (3.03) | 126 (27.99) | 240 (72.01) | |
| Others | 441 (3.21) | 158 (38.21) | 283 (61.79) | |
| Media exposure | P<0.001 | |||
| No | 5,873 (61.71) | 1,342 (20.76) | 4,531 (79.24) | |
| Yes | 3,951 (38.29) | 1,913 (40.06) | 2,038 (59.94) | |
| Wealth quintiles | P<0.001 | |||
| Poorest | 2,907 (19.10) | 497 (13.88) | 2,410 (86.12) | |
| Poorer | 1,499 (20.29) | 321 (17.27) | 1,178 (82.73) | |
| Middle | 1,359 (20.12) | 343 (21.08) | 1,016 (78.92) | |
| Richer | 1,316 (19.56) | 469 (32.15) | 847 (67.85) | |
| Richest | 2,743 (20.93) | 1,625 (54.77) | 1,118 (45.23) | |
| Religion | P<0.001 | |||
| Orthodox | 3,535 (40.49) | 1,517 (40.22) | 2,018 (59.78) | |
| Protestant | 1,784 (22.39) | 456 (21.72) | 1,328 (78.28) | |
| Muslim | 4,318 (34.63) | 1,250 (19.37) | 3,068 (80.63) | |
| Others | 187 (2.49) | 32 (11.71) | 155 (88.29) | |
| Parity | P<0.001 | |||
| No | 985 (8.54) | 442 (39.68) | 543 (60.32) | |
| 1-2 | 2,949 (27.72) | 1,204 (34.70) | 1,745 (65.30) | |
| 3-4 | 2,343 (24.23) | 764 (27.99) | 1,579 (72.01) | |
| 5+ | 3,547 (39.51) | 845 (21.16) | 2,702 (78.84) | |
| Family size | P<0.001 | |||
| <5 | 3,653 (34.59) | 1,447 (34.52) | 2,206 (65.48) | |
| >=5 | 6,171 (65.41) | 1,808 (24.78) | 4,363 (75.22) | |
| Sex of Head of Household | P=0.0642 | |||
| Male | 7,914 (87.24) | 2,583 (27.62) | 5,331 (72.38) | |
| Female | 1,910 (12.76) | 672 (31.74) | 1,238 (68.26) | |
| Native language | P<0.001 | |||
| Amarigna | 4,024 (40.09) | 1,753 (42.18) | 2,271 (57.82) | |
| Tigregna | 1,001 (6.49) | 401 (40.76) | 600 (59.24) | |
| Oromigna | 2,281 (37.05) | 526 (13.38) | 1,755 (86.62) | |
| Afarigna | 441 (0.49) | 80 (17.90) | 361 (82.10) | |
| Somaligna | 618 (1.95) | 179 (27.25) | 439 (72.75) | |
| Sidamigna | 236 (4.23) | 49 (18.73) | 187 (81.27) | |
| Agniwakigna | 112 (0.04) | 33 (36.80) | 79 (63.20) | |
| Nuwerigna/Gambeligna | 193 (0.04) | 34 (20.01) | 159 (79.99) | |
| Gumuzigna/Bangagna | 144 (0.31) | 16 (11.56) | 128 (88.44) | |
| Others | 774 (9.31) | 184 (23.25) | 590 (76.75) | |
| Decision making | P<0.001 | |||
| No | 2,952 (29.45) | 695 (23.01) | 2,257 (76.99) | |
| Yes | 6,872 (70.55) | 2,560 (30.29) | 4,312 (69.71) | |
| Wife-beating | P<0.001 | |||
| Accept | 5,931 (66.86) | 1,521 (22.61) | 4,410 (77.39) | |
| Refuse | 3,893 (33.14) | 1,734 (39.33) | 2,159 (60.67) | |
| Place of residence | P<0.001 | |||
| Urban | 2,491 (16.22) | 1,474 (59.32) | 1,017 (40.68) | |
| Rural | 7,333 (83.78) | 1,781 (22.11) | 5,552 (77.89) | |
| Region | P<0.001 | |||
| Tigray | 957 (6.44) | 359 (39.01) | 598 (60.99) | |
| Afar | 866 (0.94) | 241 (30.45) | 625 (69.55) | |
| Amhara | 1,128 (23.61) | 498 (45.09) | 630 (54.91) | |
| Oromia | 1,317 (39.00) | 205 (15.65) | 1,112 (84.35) | |
| Somali | 978 (3.16) | 272 (26.37) | 706 (73.63) | |
| Benishangul | 806 (1.11) | 178 (21.89) | 628 (78.11) | |
| SNNPR | 1,217 (21.25) | 283 (23.26) | 934 (76.74) | |
| Gambela | 712 (0.29) | 236 (39.30) | 476 (60.70) | |
| Harari | 576 (0.24) | 390 (68.03) | 186 (31.97) | |
| Addis Ababa | 677 (3.47) | 439 (62.95) | 238 (37.05) | |
| Dire Dawa | 590 (0.49) | 154 (25.21) | 436 (74.79) | |
| Community literacy level | P<0.001 | |||
| Low | 3,987 (36.46) | 749 (14.64) | 3,238 (85.36) | |
| Medium | 3,425 (42.88) | 1,110 (27.03) | 2,315 (72.97) | |
| High | 2,412 (20.66) | 1,396 (54.30) | 1,016 (45.70) | |
| Community socioeconomic level | P<0.001 | |||
| Low | 4,629 (45.25) | 874 (17.51) | 3,755 (82.49) | |
| Moderate | 2,604 (35.99) | 892 (28.31) | 1,712 (71.69) | |
| High | 2,591 (18.76) | 1,489 (53.51) | 1,102 (46.49) | |
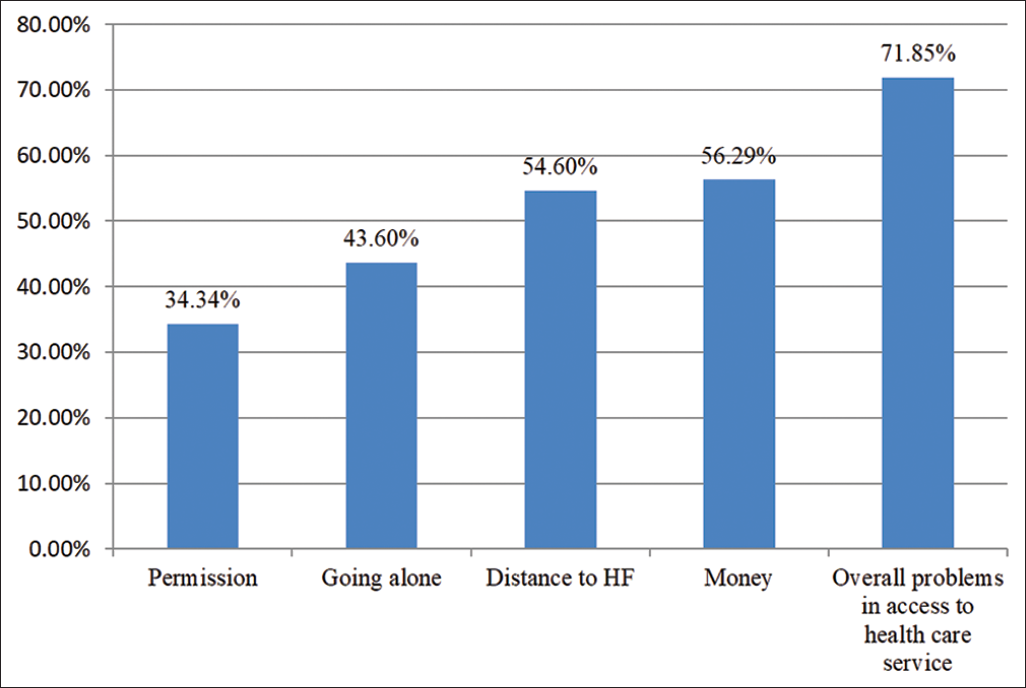
Figure 1 shows the barriers to access health care services in Ethiopia. Approximately 71.9% of married women reported having at least one barrier to accessing health care services and the most stated barrier, as indicated by 56.3% of respondents, was money. Approximately 54.6%, 43.6%, and 34.3% of respondents reported that distance to a health facility, going alone, and receiving permission were barriers to accessing health care services, respectively.
- Barriers in access to health care services among married women in Ethiopia: evidence from 2016 EDHS
Table 1 also outlines the barriers in accessing health care services by sociodemographic characteristics. More than three-quarters (78.2%) of women who had no formal education reported barriers to accessing health care services compared to less than one-third (36.5%) with higher education. Socioeconomic inequalities in access to health care services revealed 86.1% of women in the poorest wealth index reporting barriers.
Individual- and Community-level Factors Associated with Barriers to Accessing Health Care Services among Married Women in Ethiopia
The random effects of the individual- and community factors associated with barriers to health care services access are presented in Table 2. Model 0 showed significant variation in the odds of reporting barriers in access to health care service across the clusters (σ2=2.24, 1.82-2.74). Approximately 43% of the total variance in barriers to accessing health care services were attributed to between- cluster variations, as shown by the Intra-Cluster Correlation (ICC=0.43). This estimate decreased by 17% in Model I, 6% (ICC=0.20) in Model II, and 1% in Model III (ICC=0.19). The variations in the odds of facing barriers to health care accessibility were highly attributed to the variances in the clustering at the primary sampling units. Akaike's Information Criterion (AIC) values showed a decrement in the individual- and community model, revealing Model III as the best-fitted model.
| Random effect result | Model 0 | Model I | Model II | Model III |
|---|---|---|---|---|
| PSU variance (95% CI) | 2.24 (1.82-2.74) | 1.14 (0.89-1.47) | 0.89 (0.70-1.14) | 0.92 (0.71-1.19) |
| ICC | 0.43 | 0.26 | 0.20 | 0.19 |
| LR Test | 1905.46 | 711.45 | 501.08 | 422.92 |
| Wald chi-square and p-value | reference | 423.99 | 471.31 | 720.62 |
| Model fitness | ||||
| Log-likelihood | -4941.0641 | -4623.6947 | -4759.642 | -4555.8912 |
| AIC | 9886.128 | 9341.389 | 9553.284 | 9235.782 |
| PSU | 643 | 643 | 643 | 643 |
| N | 9,824 | 9,824 | 9,824 | 9,824 |
PSU - Primary Sampling Unit; ICC - Intra-Cluster Correlation; LR Test - Likelihood Ratio Test; AIC - Akaike's Information Criterion
Table 3 outlines the fixed effects models of the individual- and community-level factors associated with barriers to accessing health care services. Controlling for exploratory factors, the results showed that women with secondary education had the lowest odds of reporting health care service access barriers (aOR=0.49, 95% CI: 0.320.77) compared to those with no formal education. Women whose occupation was sales (aOR=0.73, 95% CI: 0.56-0.95) were less likely to report barriers compared to respondents who were unemployed.
| Variables | Model I | Model II | Model III |
|---|---|---|---|
| Women educational level | |||
| No formal education (Reference) | |||
| Primary school | 0.90 (0.72-1.11) | 0.88 (0.71-1.09) | |
| Secondary school | 0.48 (0.31-0.76)** | 0.49 (0.32-0.77)** | |
| Higher | 0.73 (0.41-1.30) | 0.74 (0.42-1.31) | |
| Husband educational level | |||
| No formal education (Reference) | |||
| Primary school | 0.87 (0.68-1.10) | 0.83 (0.65-1.05) | |
| Secondary school | 0.83 (0.59-1.17) | 0.79 (0.56-1.11) | |
| Higher | 0.62 (0.37-1.05) | 0.61 (0.36-1.01) | |
| Women occupation | |||
| Not working (Reference) | |||
| Professional or technical or managerial | 0.85 (0.43-1.67) | 0.86 (0.44-1.68) | |
| Clerical | 0.28 (0.06-1.16) | 0.29 (0.06-1.27) | |
| Sales | 0.74 (0.57-0.97)* | 0.73 (0.56-0.95)* | |
| Agricultural employee | 1.07 (0.80-1.43) | 1.11 (0.83-1.49) | |
| Services | 1.17 (0.64-2.14) | 1.11 (0.60-2.03) | |
| Skilled manual | 0.85 (0.51-1.43) | 0.89 (0.53-1.49) | |
| Unskilled manual | 1.31 (0.72-2.38) | 1.29 (0.70-2.36) | |
| Others | 0.47 (0.28-0.79)** | 0.46 (0.26-0.80) | |
| Husband occupation | |||
| Not working (Reference) | |||
| Professional or technical or managerial | 1.16 (0.73-1.85) | 1.23 (0.77-1.96) | |
| Clerical | 1.13 (0.47-2.73) | 1.34 (0.56-3.22) | |
| Sales | 1.01 (0.66-1.53) | 1.07 (0.70-1.63) | |
| Agricultural employee | 0.91 (0.67-1.23) | 0.95 (0.70-1.29) | |
| Services | 1.03 (0.59-1.78) | 1.16 (0.68-1.99) | |
| Skilled manual | 1.02 (0.70-1.47) | 1.09 (0.75-1.58) | |
| Unskilled manual | 0.88 (0.54-1.43) | 0.98 (0.60-1.59) | |
| Others | 1.09 (0.66-1.80) | 1.17 (0.70-1.95) | |
| Economic status | |||
| Poorest (Reference) | |||
| Poorer | 0.76 (0.57-1.01) | 0.80 (0.60-1.06) | |
| Middle | 0.74 (0.53-1.01) | 0.80 (0.58-1.11) | |
| Richer | 0.41 (0.29-0.58)*** | 0.46 (0.32-0.65)*** | |
| Richest | 0.26 (0.17-0.39)*** | 0.34 (0.22-0.54)*** | |
| Media exposure | |||
| No (Reference) | |||
| Yes | 0.80 (0.64-1.01) | 0.80 (0.63-1.01) | |
| Religion | |||
| Orthodox (Reference) | |||
| Protestant | 1.31 (0.95-1.80) | 1.00 (0.71-1.41) | |
| Muslim | 0.77 (0.55-1.08) | 0.67 (0.47-0.96)* | |
| Others | 2.17 (0.91-5.15) | 1.61 (0.66-3.89) | |
| Parity | |||
| No (Reference) | |||
| 1-2 | 1.06 (0.77-1.46) | 1.05 (0.76-1.44) | |
| 3-4 | 1.20 (0.87-1.65) | 1.18 (0.85-1.63) | |
| 5+ | 1.31 (0.96-1.79) | 1.25 (0.91-1.73) | |
| Decision Making | |||
| No (Reference) | |||
| Yes | 0.91 (0.73-1.13) | 0.94 (0.75-1.17) | |
| Wife-beating | |||
| Accept (Reference) | |||
| Refuse | 0.67 (0.55-0.81)*** | 0.66 (0.55-0.81)*** | |
| Native language | |||
| Amarigna (Reference) | |||
| Tigregna | 0.62 (0.40-0.96)* | 0.45 (0.15-1.38) | |
| Oromigna | 2.56 (1.65-3.96)*** | 1.49 (0.89-2.50) | |
| Afarigna | 1.33 (0.63-2.79) | 1.47 (0.70-3.09) | |
| Somaligna | 0.93 (0.58-1.49) | 0.64 (0.35-1.17) | |
| Sidamigna | 1.02 (0.62-1.69) | 0.66 (0.40-1.07) | |
| Agniwakigna | 0.57 (0.26-1.27) | 0.52 (0.19-1.42) | |
| Nuwerigna/gambeligna | 0.88 (0.38-2.05) | 0.67 (0.28-1.60) | |
| Gumuzigna/bangagna | 1.56 (0.79-3.06) | 0.87 (0.45-1.69) | |
| Others | 0.99 (0.61-1.59) | 0.68 (0.43-1.09) | |
| Family size | |||
| <5 (Reference) | |||
| >=5 | 0.96 (0.77-1.20) | 0.94 (0.75-1.17) | |
| Place of residence | |||
| Urban (Reference) | |||
| Rural | 2.00 (1.29-3.08)** | 1.24 (0.80-1.94) | |
| Region | |||
| Tigray (Reference) | |||
| Afar | 0.94 (0.59-1.50) | 0.43 (0.14-1.30) | |
| Amhara | 0.64 (0.44-0.92)* | 0.31 (0.10-0.91)* | |
| Oromia | 4.09 (2.67-6.27)*** | 2.03 (0.64-6.36) | |
| Somali | 0.92 (0.59-1.43) | 0.77 (0.24-2.46) | |
| Benishangul | 1.81 (1.17-2.82)** | 1.13 (0.37-3.42) | |
| SNNPR | 1.52 (1.04-2.23)* | 1.21 (0.40-3.61) | |
| Gambela | 1.09 (0.72-1.63) | 0.84 (0.28-2.49) | |
| Harari | 0.27 (0.17-0.44)*** | 0.16 (0.05-0.54)** | |
| Addis Ababa | 1.16 (0.77-1.75) | 0.89 (0.30-2.60) | |
| Dire Dawa | 3.54 (2.07-6.08)*** | 2.30 (0.72-7.30) | |
| Community literacy level | |||
| Low (Reference) | |||
| Medium | 0.57 (0.41-0.80)** | 0.64 (0.45-0.92)* | |
| High | 0.34 (0.21-0.53)*** | 0.56 (0.34-0.92)* | |
| Community socioeconomic level | |||
| Low (Reference) | |||
| Moderate | 0.46 (0.34-0.62)*** | 0.62 (0.45-0.85)** | |
| High | 0.37 (0.24-0.58)*** | 0.70 (0.42-1.17) | |
Model I: model included individual-level factors; Model II: model included community-level factors; Model III (complete model): model included both individual- and community- level factors
The likelihood of reporting barriers among women in the richest (aOR=0.34, 95% CI: 0.220.54) and richer (aOR=0.46, 95% CI: 0.32-0.65) wealth index was lower compared to women in the poorest wealth index. Additionally, the odds of reporting barriers were lower among Muslim women (aOR=0.67, 95% CI: 0.47-0.96) compared to Orthodox women. The likelihood of facing barriers in accessing health care services among women who refused compared to those who accepted wifebeating was lower (aOR=0.66, 95% CI: 0.55-0.81).
The community-level factors analyzed showed region, community literacy level, and community socioeconomic status were associated with barriers to health care services access; however, place of residence (urban or rural) was not. Women in Amhara region (aOR=0.31, 95% CI: 0.10-0.91) and Harari region (aOR=0.16, 95% CI: 0.05-0.56) were less likely to report barrier access compared to women in Tigray. Women living in communities with medium (aOR=0.64, 95% CI: 0.45-0.92) and high (aOR=0.56, 95% CI: 0.34-0.92) literacy were found to report lower odds of barriers compared to those living in communities with low literacy levels. Similarly, the odds of facing barriers to health care accessibility were lower among communities of high (aOR=0.62, 95% CI: 0.45-0.85) compared to communities of low socioeconomic status.
Discussion
Discussion
Using the 2016 EDHS, we investigated the individual- and community-level factors associated with barriers to accessing health care services among married women in Ethiopia. Overall, the findings revealed that 71.8% of married women encountered at least one type of barrier (i.e., money, distance to a health facility, getting permission to go to a health facility, and going alone) to accessing health care services.
Both individual- and community-level factors were found to be linked with health care accessibility6,7,13 as seen in other sub-Saharan African countries.7,10,14,17,19 Regarding individual-level factors, we observed the likelihood of reporting barriers in access to health care services to be lower among educated women compared to those with no formal education.7,20 The influence of formal education on quality of life and overall wellbeing has been highlighted in prior studies suggesting that education enhances the freedom and decision capacity of women in matters related to their health and reproductive health services.21 Education also enhances women's awareness and health-seeking behavior, which is seen as an entry point to using health services.22
Consistent with previous work, occupation was found to be associated with health care accessibility and service utilization.23 Employed women, particularly in sales, were less likely to have barriers to accessing health care services than those who were unemployed.24 Women with higher economic status, which tends to be linked to better financial circumstances, had lower odds of reporting barriers in access to health care services.25,26 In Ethiopia, of the total health expenditure, 35.8% are out- of-pocket expenditures, and the poor may not be able to afford the costs associated with health care services utilization (i.e., transport, wasted working hours for traveling and treatment).13,26
Religion was linked to barriers in accessing health care services, similar to previous work in Africa.11 A study in Nigeria revealed that women ignored essential maternal services (i.e., skilled birth attendants), mainly due to the gender of the service provider (i.e., male).11 Working closely with religious leaders has been suggested as a mechanism to improve health care services and coverage.7,27
The results also showed that women who refused wife-beating were less likely to have barriers to access health care services than women who accepted the norm of wife-beating. A possible explanation is that women who accept wife-beating have less knowledge about their human and health rights28 On the other hand, those who refuse wife-beating are known to have higher levels of self-confidence, positive selfesteem, and capacity to utilize household resources for good health and wellbeing.29
Similar to previous work, regional variations in barriers to health care accessibility were found.7,9 In Ethiopia, huge disparities in health care access across regions were found, suggesting the unfair distribution of health care staff as a possible reason.9 Variations in the accessibility of health care across regions may also be due to differences in the quality of health services, shortage of health professionals in rural areas, and treatment approach by doctors, nurses, or other professionals.13,15
We observed that community literacy level was associated with health care accessibility. Women living in communities with literacy had lower odds of barriers in access to health care services,7 higher incomes, and availability of resources.30 Similarly, women living in communities with better socioeconomic status were less likely to face obstacles in accessing health care services.7,13 The reason may be that economically disadvantaged women may not have adequate resources to afford health services, especially in rural areas·7,13
Strengths and Limitations of the study
Our study has both strengths and limitations. One strength is that we assessed the barriers married women face in accessing health care services using nationally representative data. We also included both individual- and community-level factors for a multi-level approach. Nonetheless, there are some limitations of the study. First, a cause-effect relationship could not be established because we used cross-sectional secondary data. Second, other factors such as the perception and attitude of women towards health care accessibility were not covered due to secondary data limitations (i.e., not collected by authors).
Conclusion and Implications for Translation
This study demonstrated that more than two-thirds of married women in Ethiopia faced at least one form of barrier to accessing health care services. The findings revealed that both individual- and community-level factors such as women's education, women's occupation, economic status, religion, wifebeating attitude, region, and community literacy level, and community socioeconomic status were associated with barriers to health care accessibility.
For sustainable health development, it is important to consider multidimensional strategies and interventions to facilitate access to health care services in Ethiopia. This could be done through education, employment opportunities, and economic strengthening. In addition, equitable distribution of resources across regions and communities are key to improving health care services.
Compliance with Ethical Standards
Conflicts of interest:
The authors declare no competing interests.
Financial Disclosure:
Nothing to declare.
Ethics Approval:
This study used publicly available secondary data from the DHS Program which ensures standards are followed for the protection of respondents' privacy and confidentiality. Details regarding ethical considerations and the protection and privacy of DHS survey respondents are available at: http://goo.gl/ny8T6X. in summary, the International City Fund Institutional Review Board reviews and approves procedures and questionnaires used in DHS. It must also comply with the U.S. Department of Health and Human Services regulations for the protection of human subjections while also requiring in host country IRB approvals.
Disclaimer:
None.
Acknowledgments:
The authors thank the MEASURE DHS project for their support and for free access to the original data.
Funding/Support:
There was no funding for this study.
References
- Health Equity Brief - Access to Health Care in Allegheny County. Allegheny County Health Department; Published May 2018 (accessed )
- Is healthcare a human right? yes. Am J Med Sci. 2017;354(5):447-448.
- [CrossRef] [PubMed] [Google Scholar]
- Delivering health care to the global poor: solving the accessibility problem. Innov Technol Gov Glob. 2011;6(2):117-141.
- [CrossRef] [Google Scholar]
- Preventable deaths from lack of high-quality medical care cost trillions. ScienceDaily. Published online 2018 (accessed )
- [Google Scholar]
- Taking on the challenges of health care in Africa. Stanford Graduate School of Business. Graduate School of Stanford Business; Published June 16, 2015 (accessed )
- Determinants of women access to healthcare services in sub-saharan Africa [Abstract] Open Public Health J. 2019;12(1)
- [CrossRef] [Google Scholar]
- Breaking barriers to healthcare access: a multilevel analysis of individual- and community-level factors affecting women's access to healthcare services in Benin. Int J Environ Res Public Health. 2021;18(2)
- [CrossRef] [PubMed] [Google Scholar]
- Ethiopia's health extension program: improving health through community involvement. 2011. MEDICC Rev. 13:46-49. (accessed )
- [CrossRef] [Google Scholar]
- Availability and inequality in accessibility of health centre-based primary healthcare in Ethiopia. PLoS One. 2019;14(3):e0213896.
- [CrossRef] [PubMed] [Google Scholar]
- Empowerment and barriers to health care access among currently married women: secondary data analysis of the 201516 Myanmar demographic and health survey. DHS Program. Published June 2019 (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- Religion as a social determinant of maternal health care service utilisation in Nigeria. Afr Popul Stud. 2015;29(2)
- [CrossRef] [Google Scholar]
- What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc. Sci Med. 2006;62(4):858-865.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers and facilitating factors in access to health services in Greece. World Health Organization Regional Office for Europe; 2015. p. :174. (accessed )
- Causes and consequences of regional variations in health care. In: Pauly MV, Mcguire TG, Barros PP, eds. In: Handbook of Health Economics. Elsevier; 2011. p. :45-93. Vol 2
- [CrossRef] [Google Scholar]
- Physician Beliefs and Patient Preferences: A New Look at Regional Variation in Health Care Spending. National Bureau of Economic Research; 2013.
- [CrossRef]
- Cultural barriers to seeking care in Ethiopia: A review of the literature. 2015. Ann Glob Health. 81 (accessed )
- [CrossRef] [Google Scholar]
- Barriers in physical access to maternal health services in rural Ethiopia. BMC Health Serv Res. 2015;15(1):493.
- [CrossRef] [PubMed] [Google Scholar]
- 2016 Ethiopia Demographic and Health Survey Key Findings. CSA and ICF; 2016. p. :551.
- Analyzing barriers to accessing health care services in Holeta town, Ethiopia. Prim Health Care Open Access. 2015;05(02)
- [CrossRef] [Google Scholar]
- Utilization of maternal health-care services in Peru: the role of women's education. Health Transit Rev. 1992;2(1):49-69.
- [Google Scholar]
- Women's autonomy in health care decision-making in developing countries: a synthesis of the literature. Int J Womens Health. 2016;8:191-202.
- [CrossRef] [PubMed] [Google Scholar]
- Inequities in utilization of reproductive and maternal health services in Ethiopia. Int J Equity Health 2017:16.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of the use of maternal health services in rural Bangladesh. Health Promot Int. 2003;18(4):327-337.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of type of employment on women's use of prenatal-care services and family planning in urban Cebu, the Philippines. Stud Fam Plann. 1998;29(1):69-78.
- [CrossRef] [PubMed] [Google Scholar]
- Health care financing reform in Ethiopia: improving quality and equity. USAID; 2012. p. :12. (accessed )
- 2017. Primary Health Care Systems (PRIMASYS): Case Study from Ethiopia. WHO; :36. (accessed )
- The role of faith leaders in influencing health behaviour: a qualitative exploration on the views of Black African Christians in Leeds, United Kingdom. Pan Afr Med J. 2018;30:199.
- [CrossRef] [PubMed] [Google Scholar]
- Women's attitude towards wifebeating and its relationship with reproductive healthcare seeking behavior: A countrywide population survey in Bangladesh. PLoS One. 2018;13(6):e0198833.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal behavior and experience, care access, and agency as determinants of child diarrhea in Bolivia. 2010. Rev Panam Salud Publica Pan Am J Public Health. 28:429-439. (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- What are the effects of education on health. In: Desjardins R, Schuller T, eds. Measuring the Effects of Education on Health and Civic Engagement. Proceedings of the Copenhagen Symposium. OECD; 2006. p. :171-310.
- [Google Scholar]





