Translate this page into:
Racial/Ethnic Disparities in Temporal Trends of Myocardial Infarction Hospitalizations Among Pregnant Women in the United States: 2009-2018
Abstract
There has been an increase in the incidence of Myocardial Infarction (MI) among pregnant women in the United States. There have been no studies examining the trends in the rates of gestational MI hospitalizations by race/ethnicity;and therefore, we undertook this study. No prior studies have examined the trends in the rates of gestational MI hospitalizations by race and ethnicity. In this study, we examined temporal trends of MI-related hospitalizations among pregnant women using the Nationwide Inpatient Sample (NIS) dataset from 2009 to 2018. We performed joinpoint regression analyses to assess trends in the rates of MI by race/ethnicity during the study period. Overall, there was an increase in the rates of MI among pregnant women during the study period (from 9.7 per 100,000 hospitalizations in 2009 to 18.1 per 100,000 hospitalizations in 2018) with an average annual percentage change (AAPC) of 7.2, (95% Confidence Interval (CI)=[4.0, 10.5]. The overall rate of MI was highest in non-Hispanic (NH)-Blacks and the greatest increments in rates of MI- related hospitalizations were noted in NH-Blacks during 2013-2018, and in Hispanics during the entire study period (2009-2018). NH-Blacks and Hispanics bear a disproportionately high burden of MI among pregnant women in the US. More worrisome is the first-ever reported finding in this study of a widening Black-White disparity in MI-related hospitalizations over the past decade.
Keywords
Myocardial Infarction
Temporal Trends
Racial Disparity
Pregnancy
Joinpoint Regression
Nationwide Inpatient Sample Database
Introduction
In the United States (US), despite an overall 48.7% decrease in hospitalization rates for myocardial infarctions (MI) between 2000 and 2014,1 the incidence of MI among pregnant women has been on the rise. From 2005 to 2014, the rate of gestational MI was reported to have increased by 18.9% with the frequency of acute MI noted to be 8.7 per 100,000 pregnancies.2 Due to rising rates of gestational MI2 while rates decreased in the general population,1 it is essential to examine gestational MI trends as trends of the general population may not be indicative of MI trends among pregnant women. Therefore, although disparities in MI trends by race in the general population have been reported,1 gestational MI trends must be analyzed to determine if this disparity is also observed among pregnant women.
When stratified by race, significant variance in cardiovascular disease outcomes among pregnant women has been observed. Between 2007 and 2017, Non-Hispanic (NH)-Black pregnant women were 1.23 (95% CI: 1.06-1.42) times more likely than their White counterparts to experience an acute MI.3 While previous studies have reported on higher incidence of acute MI among NH-Black pregnant women,3,4 to our knowledge, no study has investigated changes in the rates of MI by race/ethnicity. Examining these temporal trends are important in detecting improvement or otherwise in closing the racial/ethnic disparities in the incidence of MI in pregnant women. To address this knowledge gap, we analyzed temporal trends of MI incidence by race and ethnicity among hospitalized pregnant women over the previous decade (2009 to 2018) in the US.
Methods
This cross-sectional study was conducted using the Nationwide Inpatient Sample (NIS)5 dataset for the years 2009-2018. NIS is the largest all-payer inpatient database in the US. Each year, the dataset retrieves information on hospitalizations occurring in 47 states in the US, and when weighted, corresponds to about 35 million annual hospitalizations. All pregnancy related hospitalizations in women aged 15-49 years were included in this study. NIS used International Classification of Diseases, Ninth and Tenth Revision, Clinical Modification (ICD-09- CM and ICD-10-CM) codes to capture the diagnoses and procedures associated with each hospitalization. Myocardial infarction (outcome for this study) was identified using ICD-09-CM diagnosis codes starting with 410, and ICD-10-CM diagnosis codes starting with 121, 122 and 123 in patients' hospitalization discharge records. Race/ethnicity was categorized into non- Hispanic (NH) White, NH-Black and Hispanic. Joinpoint regression, a novel technique for determining the trend of the outcome (MI) over time, was utilized. Joinpoint regression assumes zero joinpoint (straight line) to initially fit the outcome over time; and then iteratively adds singular increments of joinpoints (change in trend) till statistically significant model with optimal joinpoints is achieved through Monte Carlo simulation.6,7 We created joinpoint regression models for the overall pregnant population and then among individual racial/ethnic categories. Average annual percentage change (AAPC) and 95% confidence intervals (CI) were generated from these models, which demonstrated the level of change in the incidence of MI. We used two-tailed hypothesis testing for all statistical analyses, and the type-1 error rate was set at 5%. We utilized R version 3·5·l (University of Auckland, Auckland, New Zealand) and RStudio Version 1·1·5001 (Boston, MA) for performing all statistical analyses. The study was performed on de-identified publicly available data and therefore, was granted an exempt status by the Institutional Review Board at Baylor College of Medicine.
Results
During the study period of 2009-2018, we evaluated a total of 45,498,605 pregnancy-related hospitalizations. Out of these, 5,031 (11.1 per 100,000 hospitalizations) had MI. Among NH- Whites, there were 2,031 hospitalizations with MI, out of the total 21,942,100 pregnancy-related hospitalizations (9.3 per 100,000 hospitalizations); among NH-Blacks, there were 1,447 hospitalizations with MI, out of the total 6,549,906 pregnancy hospitalizations (22.1 per 100,000 hospitalizations). Among Hispanics, MI corresponded to 716 out of 9,017,320 pregnancy-related hospitalizations (7.9 per 100,000 hospitalizations).
Figure 1 illustrates the rates of MI per 100,000 pregnancy-related hospitalizations in the US during the study period by race/ethnicity. We detected an overall increase in the rates of MI during the study period with an AAPC of 7.2% (95% CI [4.0, 10.5], p<0.05). Among NH-Blacks, there was an 8.4% average annual increase in the rates of MI (95% CI: [0.5, 18.4], p<0.05) and Hispanics had an AAPC of 12.6% (95% CI [1.7, 24.5], p<0.05). The rates for NH- Whites did not change (p>0.05) during the study period. It was observed that NH-Black pregnant women had increased rates of MI throughout the study duration when compared to their NH-White and Hispanic counterparts, and the Black-White disparity widened greatly during the 2013-2018 period, with the MI rates for NH-Blacks being twice that of NH-Whites in 2013 and the difference quadrupling by 2018.
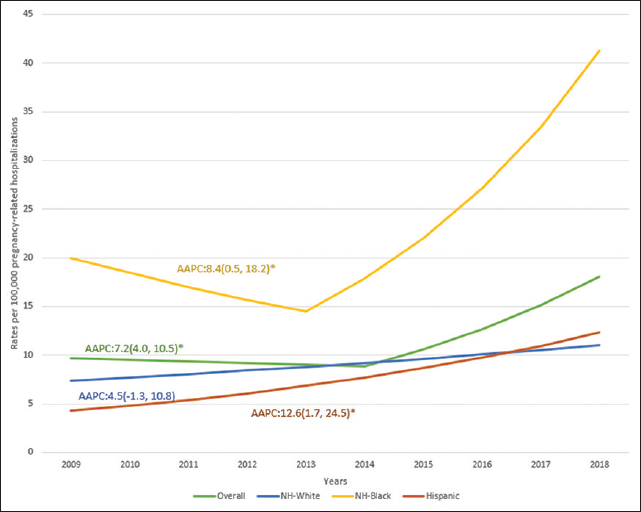
- Trends in the rates of myocardial infarction in preg- nancy related hospitalizations among different race/ethnicities in the US: 2009-2018.
Discussion, Conclusion and Implications for Translation
Our results coincide with previous study that observed an increase in gestational MI rates over time.2 Moreover, our results are also in agreement with studies that reported higher rates of MI among NH-Black pregnant women.2,3 Our study also showed that the rate of increase in MI incidence was highest in NH-Black and Hispanic pregnant women. A possible explanation for this observation could be that NH-Blacks and Hispanics have been reported to have higher rates of obesity;6,8 as another study noted that cardiovascular risk factors such as hypertension, diabetes, and obesity may be responsible for the higher acute MI rates in NH-Black pregnant women.4 However, further research is needed to explain why the disparity in MI is widening.
Our study is valuable since it depicts the increase in MI incidence in the overall pregnant hospitalized population, with higher increment in Hispanics and NH-Blacks. Moreover, the observed disparity in MI rates signifies the need for the healthcare system to address this trend. To potentially curb the increasing rates of MI on a widespread scale, educational outreach programs on MI and its risk factors should be implemented, particularly in minority communities. At the individual level, healthcare providers should emphasize the significance of cardiovascular risk factors on MI to pregnant women and the actions/ care needed to eliminate those risk factors. Providers should also provide culturally aligned consultations when addressing risk factors among racial/ethnic minority pregnant women in order to augment uptake of prescribed recommendations.
Compliance with Ethical Standards
Conflicts of interest:
None.
Financial Disclosure:
None.
Ethics Approval:
The study was approved as exempt by the Institutional Review Board of Baylor College of Medicine.
Disclaimer:
None
Acknowledgments:
None
Funding/Support:
Research funding support was provided by the U.S. Department of Health and Human Services and Health Resources and Services Administration for Baylor College of Medicine Center of Excellence in Health Equity, Training, and Research (Grant No: D34HP31024).
References
- Trends in acute myocardial infarction by race and ethnicity. J Am Heart Assoc. 2020;9(5):e013542.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in incidence and outcomes of pregnancy-related acute myocardial infarction (From a Nationwide Inpatient Sample Database) Am J Cardiol. 2019;123(8):1220-1227.
- [CrossRef] [PubMed] [Google Scholar]
- Disparities in cardiovascular disease outcomes among pregnant and post-partum women. J Am Heart Assoc. 2021;10(1):e017832.
- [CrossRef] [PubMed] [Google Scholar]
- Acute myocardial infarction in pregnancy: a United States population-based study. Circulation. 2006;113(12):1564-1571.
- [CrossRef] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality, Rockville, MD. 2012. Healthcare Cost and Utilization Project (HCUP). (accessed )
- [Google Scholar]
- Permutation tests for joinpoint regression with applications to cancer rates [published correction appears in Stat Med 2001 Feb 28;20(4):655] Stat Med. 2000;19(3):335-351.
- [CrossRef] [Google Scholar]
- Joinpoint Regression Program, Version 4.8. 0.1 - April 2020. Bethesda, Maryland: Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute;
- [Google Scholar]
- Trends in obesity prevalence by race and hispanic origin-1999-2000 to 2017-2018. JAMA. 2020;324(12):1208-1210.
- [CrossRef] [PubMed] [Google Scholar]





